The study of matter and energy, including their interactions and behavior, forms the foundation for medical imaging techniques that use various forms of electromagnetic radiation or other energy sources to visualize internal structures of the human body. For instance, the principles of energy transfer and wave propagation are essential for understanding how X-rays interact with tissues to produce diagnostic images.
This interdisciplinary field plays a crucial role in modern healthcare, enabling non-invasive diagnosis and treatment of various medical conditions. From the discovery of X-rays by Wilhelm Conrad Rntgen in 1895 to the development of advanced imaging modalities like magnetic resonance imaging (MRI) and positron emission tomography (PET), the application of physical principles has revolutionized medical practice, improving diagnostic accuracy and patient outcomes. This foundational knowledge is indispensable for developing and refining imaging technologies, optimizing image quality, and ensuring patient safety.
The following sections will explore the core concepts underlying specific imaging modalities, delve into their clinical applications, and discuss future directions in this ever-evolving field.
Tips for Optimizing Medical Imaging Procedures
Optimizing medical imaging procedures requires a thorough understanding of the underlying physical principles and their practical application. The following tips provide guidance for enhancing image quality, minimizing radiation exposure, and improving diagnostic accuracy.
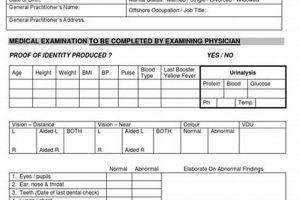
Tip 1: Proper Patient Positioning: Accurate patient positioning is crucial for acquiring diagnostically useful images. Incorrect positioning can lead to anatomical misrepresentation and obscure critical details. Precise alignment with imaging planes and the use of immobilization devices can minimize motion artifacts and ensure optimal image quality.
Tip 2: Selecting Appropriate Imaging Parameters: Careful selection of imaging parameters, such as voltage, current, and exposure time, is essential for balancing image quality and radiation dose. Optimization of these parameters based on the specific examination and patient characteristics can significantly reduce unnecessary radiation exposure while maintaining diagnostic image quality.
Tip 3: Image Quality Control: Regular quality control procedures are vital for ensuring consistent and reliable image acquisition. Evaluation of image sharpness, contrast, and noise levels helps identify potential equipment malfunctions or procedural errors, allowing for timely corrective actions.
Tip 4: Radiation Safety Practices: Adhering to established radiation safety protocols is paramount for protecting both patients and medical personnel. Implementing appropriate shielding techniques, minimizing exposure time, and optimizing imaging parameters are crucial for reducing radiation risks.
Tip 5: Continuing Education and Training: Staying abreast of the latest advancements in imaging technology and techniques is crucial for maintaining competency and delivering optimal patient care. Continuous professional development through workshops, conferences, and online resources enhances knowledge and skills in this rapidly evolving field.
Tip 6: Effective Communication: Clear communication between imaging professionals, referring physicians, and patients is essential for ensuring appropriate imaging utilization and accurate interpretation of results. Open dialogue facilitates informed decision-making and enhances patient understanding of the procedure and its potential benefits and risks.
By implementing these tips, medical imaging professionals can contribute to improved diagnostic accuracy, enhanced patient safety, and more efficient utilization of imaging resources. These practices underpin the delivery of high-quality medical imaging services.
These essential considerations underscore the importance of a comprehensive understanding of both the theoretical and practical aspects of medical imaging, paving the way for a concluding discussion on the future directions and challenges in this dynamic field.
1. Radiation Interaction
Radiation interaction forms the cornerstone of medical imaging, dictating how different tissues absorb and scatter radiation. This interaction is governed by fundamental principles of physics, including the photoelectric effect, Compton scattering, and pair production. The photoelectric effect, dominant at lower photon energies, involves the complete absorption of a photon by an atom, resulting in the ejection of an electron. This effect is heavily dependent on the atomic number of the absorbing material, explaining why bone, rich in calcium, appears brighter than soft tissue on X-ray images. Compton scattering, prevalent at higher energies, involves the scattering of a photon by an electron, resulting in a change in photon direction and energy. This process contributes to image noise and reduces image contrast. Pair production, occurring at very high energies, involves the conversion of a photon into an electron-positron pair. Understanding these interactions is crucial for optimizing imaging parameters and interpreting image contrast.
Consider, for example, the use of contrast agents in computed tomography (CT) scans. Iodine-based contrast agents exploit the photoelectric effect due to iodine’s high atomic number. The increased absorption of X-rays by iodine-enhanced tissues leads to greater contrast differentiation, allowing for better visualization of blood vessels and organs. Similarly, in mammography, the lower energy X-rays preferentially interact with denser tissues through the photoelectric effect, enabling the detection of subtle calcifications indicative of early-stage breast cancer. The energy dependence of these interactions underscores the importance of selecting appropriate radiation energies for different imaging modalities and patient characteristics.
A comprehensive understanding of radiation interaction is fundamental for developing new imaging techniques, optimizing image quality, minimizing radiation dose, and accurately interpreting medical images. Challenges remain in further refining our understanding of these complex interactions, particularly in heterogeneous tissues. This knowledge, however, remains essential for advancing the field of medical imaging and improving patient care.
2. Image Formation
Image formation in medical imaging relies heavily on principles of physics. The process involves acquiring signals generated by the interaction of energy (e.g., X-rays, ultrasound waves, radio waves) with body tissues, and subsequently reconstructing these signals into diagnostically useful images. Different imaging modalities employ distinct physical phenomena and reconstruction algorithms. In X-ray imaging, the differential attenuation of X-rays through various tissues forms the basis of image contrast. Denser tissues absorb more X-rays, appearing brighter on the image, while less dense tissues appear darker. Computed tomography (CT) utilizes multiple X-ray projections acquired from different angles, combined through sophisticated mathematical algorithms to reconstruct cross-sectional images of the body.
Magnetic Resonance Imaging (MRI) exploits the interaction of atomic nuclei with strong magnetic fields and radio waves. The specific frequencies emitted by excited nuclei provide information about their spatial location and chemical environment, allowing for the creation of detailed images of soft tissues. Ultrasound imaging utilizes high-frequency sound waves to generate images based on the reflection and scattering of these waves by tissue interfaces. The time delay and intensity of the returning echoes provide information about tissue depth and structure. Nuclear medicine techniques, such as Positron Emission Tomography (PET) and Single-Photon Emission Computed Tomography (SPECT), rely on the detection of gamma rays emitted by radiotracers administered to the patient. These techniques provide functional information about metabolic processes within the body.
Understanding the underlying physics of image formation is essential for optimizing image quality, interpreting images accurately, and developing new imaging technologies. Factors such as spatial resolution, contrast, and noise influence the diagnostic utility of medical images. Challenges in image formation include minimizing artifacts, improving signal-to-noise ratios, and developing faster and more efficient reconstruction algorithms. Continued research in physics and engineering contributes to advancements in medical imaging, enabling earlier and more accurate diagnoses, and ultimately, improved patient outcomes.
3. Instrumentation Design
Instrumentation design in medical imaging represents a crucial application of physics and directly impacts the capabilities and limitations of radiological techniques. The design of imaging equipment hinges upon fundamental principles of physics, including electromagnetism, optics, acoustics, and nuclear physics. For instance, the generation of X-rays in a CT scanner relies on precise control of electron beams and their interaction with a target material, a process governed by electromagnetic theory. Similarly, the design of MRI magnets involves intricate engineering based on principles of superconductivity and magnetic field homogeneity, ensuring consistent and high-quality image acquisition. The sensitivity and resolution of ultrasound transducers are determined by the piezoelectric properties of the materials used and the design of the acoustic lens, influencing the ability to visualize fine anatomical details.
Consider the development of multi-detector CT scanners. Advances in detector technology, coupled with faster data acquisition and processing capabilities, have significantly reduced scan times and improved spatial resolution. This translates to quicker diagnoses, reduced patient discomfort, and the ability to detect smaller lesions. Similarly, the development of phased-array ultrasound transducers, employing principles of wave interference, allows for electronic beam steering and focusing, enabling real-time three-dimensional imaging and improved diagnostic capabilities in echocardiography and obstetric ultrasound. In nuclear medicine, the design of gamma cameras with improved scintillation crystals and photomultiplier tubes has enhanced the sensitivity and spatial resolution of PET and SPECT scans, leading to more accurate detection and localization of disease processes.
The ongoing development of novel imaging technologies hinges on advancements in instrumentation design. Challenges include improving image quality while minimizing radiation dose, developing more compact and portable imaging systems, and integrating multiple imaging modalities for comprehensive diagnostic assessments. Addressing these challenges requires continued interdisciplinary collaboration between physicists, engineers, and radiologists, driving innovation and enhancing the quality of patient care through improved diagnostic capabilities and therapeutic interventions.
4. Safety Protocols
Safety protocols in radiology are intrinsically linked to the fundamental principles of physics governing the interaction of radiation with matter. These protocols are designed to minimize the potential risks associated with ionizing radiation exposure to patients, medical personnel, and the public. Understanding the physical properties of radiation, including its energy, type, and interaction mechanisms, is crucial for developing and implementing effective safety measures. The principles of radiation shielding, distance, and time form the cornerstone of radiation protection. Shielding materials, such as lead and concrete, exploit the physics of radiation absorption to attenuate the intensity of radiation beams. Increasing the distance from the radiation source reduces exposure according to the inverse square law, a fundamental principle in physics. Minimizing exposure time directly reduces the total radiation dose received.
Practical applications of these principles are evident in various radiological procedures. During fluoroscopy, lead aprons and thyroid shields are worn by medical personnel to minimize radiation exposure. In nuclear medicine, specialized handling procedures and waste disposal protocols are implemented to prevent the spread of radioactive materials. Regulations governing the design and operation of imaging equipment, such as X-ray tubes and CT scanners, incorporate physics-based safety standards to limit radiation leakage and ensure safe operating parameters. For instance, filtration materials within X-ray tubes selectively remove lower-energy photons that contribute significantly to patient dose but not to image quality. Collimation restricts the X-ray beam to the area of interest, further minimizing unnecessary exposure.
Effective implementation of safety protocols necessitates a thorough understanding of radiation physics, proper training, and adherence to established guidelines. Challenges include balancing the benefits of diagnostic imaging with the potential risks of radiation exposure, optimizing imaging parameters to minimize dose while maintaining diagnostic image quality, and ensuring compliance with evolving safety standards. Continuous advancements in imaging technology and dosimetry techniques contribute to refining safety protocols and minimizing radiation risks in medical imaging. Vigilance and adherence to these protocols are essential for ensuring the safe and effective use of medical imaging technologies, ultimately benefiting both patients and healthcare professionals.
5. Technological Advancements
Technological advancements are intrinsically linked to the evolution of physics and radiology, continually pushing the boundaries of medical imaging capabilities. These advancements stem from fundamental discoveries in physics and engineering, leading to innovative imaging modalities, improved image quality, reduced radiation doses, and enhanced diagnostic accuracy. Exploring these advancements reveals the dynamic interplay between scientific progress and clinical practice.
- Multi-Detector Computed Tomography (MDCT)
MDCT represents a significant leap forward from conventional CT scanning. Utilizing multiple detector rows, MDCT allows for faster acquisition of thinner slices, resulting in higher spatial resolution, improved image quality, and reduced scan times. This technology enables detailed visualization of complex anatomical structures, facilitating more accurate diagnoses, particularly in cardiovascular imaging and trauma assessment. Furthermore, MDCT has paved the way for advanced applications such as CT angiography and perfusion imaging.
- Hybrid Imaging Techniques (PET/CT, SPECT/CT)
Hybrid imaging systems combine the strengths of different modalities, providing both anatomical and functional information. PET/CT, for instance, integrates the metabolic information from PET with the anatomical detail of CT, enabling precise localization of disease processes, particularly in oncology and cardiology. Similarly, SPECT/CT combines the functional information from SPECT with the anatomical context of CT, enhancing diagnostic accuracy in various clinical applications, including infection imaging and bone scans.
- Magnetic Resonance Imaging (MRI) Advancements
Continuous advancements in MRI technology have expanded its diagnostic capabilities. Higher magnetic field strengths, advanced coil designs, and novel pulse sequences have led to improved spatial resolution, enhanced tissue contrast, and faster image acquisition. Techniques such as diffusion-weighted imaging (DWI) and functional MRI (fMRI) provide insights into tissue microstructure and brain function, respectively, opening new avenues for clinical research and diagnosis.
- Artificial Intelligence (AI) in Radiology
The integration of AI algorithms into radiological practice holds immense potential for enhancing image analysis, interpretation, and workflow efficiency. AI-powered tools can assist in tasks such as image segmentation, lesion detection, and automated reporting, potentially improving diagnostic accuracy and reducing radiologist workload. While still in its early stages, AI in radiology promises to transform the field by augmenting human expertise and facilitating more efficient and precise diagnostic assessments.
These technological advancements underscore the continuous evolution of medical imaging, driven by the interplay between physics, engineering, and clinical need. The ongoing development of novel imaging techniques and analysis tools promises to further refine diagnostic capabilities, improve patient outcomes, and reshape the future of radiology.
6. Diagnostic Interpretation
Diagnostic interpretation in radiology represents the culmination of the principles of physics and their application in medical imaging. Accurate interpretation relies on a thorough understanding of the underlying physical processes that generate medical images, the specific characteristics of different imaging modalities, and the potential sources of artifacts and limitations. This intricate process bridges the gap between raw image data and clinically relevant information, enabling accurate diagnoses and guiding patient management.
- Image Contrast and Tissue Characterization
Understanding how different tissues interact with various forms of energy is fundamental for interpreting image contrast. In X-ray imaging, for example, the differential attenuation of X-rays by bone, soft tissue, and air creates the contrast that allows for visualization of anatomical structures. Similarly, in MRI, the varying magnetic properties of tissues contribute to image contrast, enabling differentiation between normal and pathological tissues. Knowledge of these physical interactions is crucial for recognizing subtle differences in image intensity and texture, ultimately informing diagnostic decisions.
- Artifact Recognition and Mitigation
Artifacts, deviations from the true representation of anatomy, can arise from various sources, including patient motion, equipment limitations, and physical phenomena such as beam hardening and scattering. Recognizing and understanding the origins of artifacts is essential for accurate interpretation, preventing misdiagnosis. For instance, motion artifacts can blur or distort images, mimicking pathology. Knowledge of physics-based artifact reduction techniques, such as gating and filtering, assists in improving image quality and minimizing misinterpretations.
- Integration of Clinical Information
Diagnostic interpretation is not solely reliant on image analysis; it requires integration of clinical information, patient history, and laboratory findings. Correlating imaging findings with other clinical data provides a comprehensive understanding of the patient’s condition, enhancing diagnostic accuracy. For example, knowledge of a patient’s history of trauma can influence the interpretation of a fracture on a radiograph, distinguishing between acute and chronic injuries. Integrating clinical context with image analysis allows for more informed and personalized diagnostic assessments.
- Quantitative Image Analysis
Quantitative image analysis, involving measurements of image features such as size, shape, and intensity, provides objective data for diagnostic interpretation. This approach relies on principles of physics and mathematics to extract quantifiable information from images, enabling more precise assessment of disease progression, treatment response, and prognosis. For example, in oncology, quantitative analysis of tumor size and metabolic activity, as measured by PET scans, can inform treatment planning and monitor response to therapy.
Diagnostic interpretation represents a complex interplay between physics, technology, and clinical expertise. A strong foundation in the principles of physics and radiology is essential for accurate image analysis, artifact recognition, and integration of clinical information. As imaging technology continues to advance, the role of physics in diagnostic interpretation will remain crucial, ensuring accurate and informed clinical decision-making for improved patient care.
Frequently Asked Questions
This section addresses common inquiries regarding the intersection of physics and radiology, aiming to provide clear and concise information.
Question 1: How does physics underpin the functionality of medical imaging equipment?
Fundamental principles of physics, including electromagnetism, acoustics, and nuclear physics, govern the design and operation of medical imaging devices. For instance, X-ray generation relies on electromagnetic interactions, while ultrasound transducers utilize piezoelectric principles. Understanding these physical foundations is crucial for optimizing image quality and ensuring equipment safety.
Question 2: What is the role of physics in minimizing radiation exposure during imaging procedures?
Physics principles dictate the interaction of radiation with matter, informing safety protocols in radiology. Concepts such as shielding, distance, and time are applied to minimize radiation exposure to patients and personnel. Optimization of imaging parameters, informed by physics principles, further reduces unnecessary radiation dose.
Question 3: How does physics contribute to the interpretation of medical images?
Understanding the physical processes underlying image formation is crucial for accurate interpretation. Knowledge of how different tissues interact with energy (e.g., X-rays, ultrasound) enables radiologists to differentiate between normal and pathological findings. Physics-based image processing techniques further enhance diagnostic accuracy.
Question 4: What are some recent advancements in medical imaging driven by physics research?
Advancements in physics have led to innovations such as multi-detector CT, hybrid imaging (PET/CT, SPECT/CT), and advanced MRI techniques. These developments enhance image quality, reduce scan times, and provide more comprehensive diagnostic information, ultimately improving patient care.
Question 5: How does physics influence the development of new imaging techniques?
Discoveries in physics often pave the way for new imaging modalities. For example, advancements in detector technology and data processing have revolutionized CT and MRI. Ongoing research in areas such as nanotechnology and biophysics promises to further transform medical imaging in the future.
Question 6: What is the importance of physics education for radiologists and medical physicists?
A strong foundation in physics is essential for both radiologists and medical physicists. This knowledge enables them to understand the principles behind image acquisition, optimize imaging protocols, interpret images accurately, and ensure patient safety in the context of rapidly evolving imaging technologies.
A thorough understanding of the physics underpinning radiology is fundamental for advancing the field, optimizing imaging procedures, and ultimately, improving patient care. Continued exploration of these principles will drive innovation and enhance diagnostic capabilities in the years to come.
Further sections will explore specific applications of physics in various imaging modalities and discuss the future directions of research and development in this dynamic field.
Conclusion
The exploration of the interplay between physics and radiology reveals a foundational relationship crucial for advancing medical imaging. From the fundamental principles governing radiation interactions and image formation to the intricate design of imaging instrumentation and the development of robust safety protocols, physics underpins every facet of this field. Technological advancements, driven by continuous research and development, demonstrate the transformative power of applying physical principles to improve diagnostic capabilities, enhance image quality, and minimize risks. Accurate diagnostic interpretation, the cornerstone of effective patient care, relies heavily on a thorough understanding of these underlying physical processes, enabling clinicians to extract clinically relevant information from complex image data. The synergy between physics and radiology is further exemplified by the integration of quantitative image analysis and the ongoing development of artificial intelligence tools, promising to reshape the future of medical imaging.
The continuous evolution of medical imaging necessitates ongoing exploration and refinement of the physical principles that govern this field. Continued interdisciplinary collaboration between physicists, engineers, and radiologists is essential for driving innovation, developing novel imaging technologies, and optimizing existing methodologies. This dedication to advancing the intersection of physics and radiology holds the key to unlocking further improvements in diagnostic accuracy, personalized medicine, and ultimately, better patient outcomes worldwide.