Restorative treatment for injuries and illnesses involving exercises, manual therapy, and other modalities is available in the Roseburg area. These services aim to improve mobility, reduce pain, and restore function to individuals affected by various conditions, from acute injuries like sprains and fractures to chronic conditions such as arthritis and back pain. A qualified practitioner typically develops a personalized plan to address specific patient needs and goals.
Regaining lost physical function and independence offers significant improvements to quality of life. Restorative movement allows individuals to participate more fully in daily activities, work, and recreational pursuits. This type of care emphasizes patient education and self-management strategies to promote long-term wellness and prevent future issues. Historically, the field has evolved significantly with advancements in medical technology and research, leading to more effective and specialized interventions.
This information provides context for exploring specific aspects of rehabilitation services within the Roseburg community. Subsequent sections will delve into available services, practitioner specializations, and the process of accessing care within this region.
Tips for Optimizing Recovery
Maximizing the benefits of rehabilitative care involves active patient participation and adherence to recommended practices. The following tips offer guidance for optimizing recovery and achieving optimal functional outcomes.
Tip 1: Consistent Adherence to Treatment Plans: Following prescribed exercises and attending scheduled sessions diligently is crucial for consistent progress. Consistent engagement with the treatment plan facilitates a more efficient and effective recovery.
Tip 2: Open Communication with Healthcare Providers: Clear and consistent communication with practitioners regarding pain levels, progress, and any concerns allows for adjustments to the treatment plan as needed, ensuring its continued effectiveness and patient comfort.
Tip 3: Maintaining a Healthy Lifestyle: Supporting the recovery process through proper nutrition, adequate sleep, and stress management techniques contributes to overall well-being and enhances the body’s healing capacity.
Tip 4: Setting Realistic Goals: Collaborating with practitioners to establish achievable and measurable goals provides motivation and a framework for tracking progress, promoting a positive and encouraging rehabilitation experience.
Tip 5: Gradual Return to Activity: Avoiding overexertion and gradually increasing activity levels as advised helps prevent setbacks and allows the body to adapt safely to increasing demands.
Tip 6: Active Participation in Home Exercise Programs: Regularly performing prescribed home exercises reinforces gains made during therapy sessions and accelerates the recovery process.
Tip 7: Understanding the Importance of Rest and Recovery: Allowing adequate time for rest and recovery between exercise sessions is essential for tissue healing and preventing injury, optimizing the overall effectiveness of the rehabilitation process.
By following these guidelines, individuals undergoing rehabilitation can actively contribute to their recovery journey and enhance their chances of achieving optimal functional outcomes. These practices empower patients to regain independence and improve their overall quality of life.
Understanding these key elements of successful rehabilitation prepares individuals for a more informed and proactive approach to their care. The following section offers a concluding perspective on the significance of seeking professional guidance for achieving optimal health and well-being.
1. Qualified Practitioners
The efficacy of restorative treatment in Roseburg, Oregon, is directly linked to the expertise of qualified practitioners. These professionals possess the necessary education, licensure, and clinical experience to accurately assess, diagnose, and develop effective treatment plans for patients seeking relief from pain and restoration of function. Their understanding of anatomy, physiology, and biomechanics, combined with specialized knowledge in therapeutic exercise, manual therapy, and other modalities, forms the foundation of successful patient outcomes. For instance, a practitioner’s ability to accurately diagnose the root cause of lower back pain, whether stemming from a herniated disc or muscle strain, will directly influence the chosen treatment approach and the patient’s likelihood of experiencing relief.
Qualified practitioners in this field play a vital role in patient education and self-management. They empower individuals to actively participate in their recovery by providing clear instructions, demonstrating proper exercise techniques, and offering guidance on lifestyle modifications that support long-term health and wellness. Consider a patient recovering from a knee injury; the guidance of a qualified practitioner can be instrumental in ensuring proper rehabilitation, preventing re-injury, and restoring optimal joint function. Furthermore, these practitioners are adept at adapting treatment plans to the unique needs of each individual, considering factors such as age, overall health, and specific functional goals. This personalized approach is essential for achieving optimal outcomes and maximizing the effectiveness of interventions.
In summary, access to qualified practitioners is essential for individuals in Roseburg seeking effective restorative treatment. Their specialized knowledge, clinical skills, and commitment to patient-centered care directly contribute to successful outcomes and contribute significantly to the overall health and well-being of the community. Finding a provider with appropriate credentials and experience is a crucial step in the rehabilitation process. Further investigation regarding specific specializations and professional certifications can enhance patient understanding and inform decision-making when selecting a practitioner.
2. Individualized Treatment Plans
Effective rehabilitation in Roseburg relies heavily on individualized treatment plans. A standardized approach to care fails to address the unique circumstances and specific needs of each individual. Factors such as the type and severity of injury, pre-existing health conditions, lifestyle, and personal goals necessitate a tailored approach. For example, a treatment plan for a young athlete recovering from a sports-related injury will differ significantly from a plan designed for an older adult managing chronic arthritis. Individualized plans consider these variations, optimizing outcomes through targeted interventions.
Developing an individualized plan typically begins with a comprehensive assessment conducted by a qualified practitioner. This assessment evaluates the patient’s current functional limitations, pain levels, range of motion, strength, and other relevant factors. The practitioner considers the patient’s medical history, lifestyle, and personal goals to formulate a tailored program. This program may include specific exercises, manual therapy techniques, modalities like ultrasound or electrical stimulation, and patient education regarding self-management strategies. For instance, a patient recovering from a shoulder injury might receive a plan incorporating exercises to improve range of motion and strengthen supporting muscles, manual therapy to address joint restrictions, and education on proper posture and body mechanics to prevent future problems.
The practical significance of individualized treatment plans is evident in improved patient outcomes. Tailored interventions lead to more effective pain management, faster recovery times, and greater functional restoration. Moreover, individualized plans empower patients by actively involving them in their rehabilitation journey. By understanding the rationale behind their treatment and actively participating in its implementation, patients are more likely to adhere to the plan and achieve their desired goals. This approach fosters a collaborative relationship between patient and practitioner, enhancing motivation and ultimately contributing to successful rehabilitation outcomes.
3. Evidence-based techniques
Effective physical therapy in Roseburg relies on the application of evidence-based techniques. These techniques are grounded in scientific research and clinical trials demonstrating their efficacy in treating specific conditions. This approach ensures that interventions are not only theoretically sound but also demonstrably effective in producing positive patient outcomes. Utilizing evidence-based practices minimizes the risk of applying ineffective or potentially harmful treatments. For instance, a practitioner might choose a specific exercise protocol for a patient with knee osteoarthritis based on research demonstrating its effectiveness in reducing pain and improving function. This informed decision-making, rooted in scientific evidence, maximizes the likelihood of a successful outcome. Conversely, relying on anecdotal evidence or outdated practices could lead to suboptimal results or even exacerbate existing issues. The commitment to evidence-based care reflects a dedication to providing the highest quality, most effective interventions available.
The practical significance of this approach is reflected in several ways. Patients benefit from improved outcomes, shorter recovery times, and reduced risk of complications. Evidence-based techniques ensure care aligns with the latest scientific understanding of effective rehabilitation strategies. For example, the use of manual therapy techniques supported by research demonstrating their effectiveness in improving joint mobility and reducing pain illustrates this point. Moreover, the reliance on objective evidence promotes transparency and accountability within the field. Practitioners utilizing evidence-based techniques demonstrate a commitment to professional development and staying abreast of advancements in the field. This ongoing pursuit of knowledge benefits both patients and the profession by ensuring best practices are consistently implemented.
In summary, the integration of evidence-based techniques within physical therapy in Roseburg is crucial for delivering high-quality care and achieving optimal patient outcomes. This reliance on scientific evidence underscores a commitment to providing effective, safe, and scientifically validated interventions. The ongoing evaluation and incorporation of new research findings into practice ensures patients receive the most advanced and effective care available, contributing to improved health and well-being within the community. This commitment to evidence-based practice distinguishes quality care and empowers both patients and practitioners with the knowledge necessary for successful rehabilitation outcomes.
4. Comprehensive Assessments
Thorough evaluations are essential to effective restorative treatment in Roseburg. These assessments provide the foundation for developing individualized treatment plans that address specific patient needs and goals. A comprehensive assessment goes beyond simply identifying the immediate source of pain or dysfunction; it delves into the underlying factors contributing to the individual’s condition. This holistic approach ensures that treatment addresses the root cause of the problem, not just the symptoms, promoting long-term health and well-being. The following facets illustrate the key components of a comprehensive assessment within this context.
- Medical History Review
A detailed review of medical history provides crucial context for understanding a patient’s current condition. Prior injuries, surgeries, chronic illnesses, and family history can all influence the development and progression of musculoskeletal issues. For example, a patient with a history of diabetes may experience slower healing times, requiring adjustments to the treatment plan. Similarly, previous injuries can create biomechanical imbalances that predispose an individual to further problems. Understanding this history allows practitioners to tailor interventions, avoid contraindicated treatments, and develop strategies that address both current and potential future issues.
- Physical Examination
A thorough physical examination provides objective data regarding a patient’s current physical state. This includes assessing posture, range of motion, strength, flexibility, and neurological function. For instance, observing a patient’s gait can reveal imbalances or compensations that contribute to pain or dysfunction. Palpating muscles and joints helps identify areas of tenderness, inflammation, or restricted movement. Specific orthopedic tests may be performed to assess ligament stability or identify potential nerve impingements. These findings, combined with the patient’s subjective reports of pain and functional limitations, provide a comprehensive picture of their physical capabilities and limitations.
- Functional Movement Analysis
Evaluating how a patient performs everyday movements provides insights into functional limitations and movement patterns that may contribute to their condition. Observing activities such as squatting, lifting, walking, or reaching can reveal movement compensations, muscle imbalances, and limitations in range of motion. For example, a patient with lower back pain might exhibit limited hip mobility during a squat, indicating a potential contributing factor to their discomfort. Analyzing these functional movements informs the development of targeted exercises and interventions that address specific movement impairments and improve overall functional capacity.
- Goal Setting and Patient Education
A critical aspect of comprehensive assessments involves collaborative goal setting and patient education. Understanding a patient’s individual goals, whether returning to a specific sport, managing chronic pain, or improving daily activities, informs the development of a targeted treatment plan. Educating patients about their condition, the rationale behind the chosen interventions, and their role in the recovery process empowers them to actively participate in their rehabilitation. This collaborative approach fosters a stronger therapeutic alliance, enhances patient motivation, and promotes better adherence to the prescribed treatment plan, ultimately leading to improved outcomes.
These integrated facets of comprehensive assessments ensure personalized treatment plans within restorative treatment in Roseburg. By thoroughly understanding each patient’s individual circumstances, needs, and goals, practitioners can develop effective interventions that address the root causes of dysfunction and promote optimal recovery. This holistic approach not only resolves immediate symptoms but also equips individuals with the knowledge and tools necessary to maintain long-term health, well-being, and prevent future issues.
5. State-of-the-art Facilities
Access to advanced facilities plays a significant role in the effectiveness of restorative treatment within Roseburg. Modern equipment and specialized environments contribute directly to improved patient outcomes and enhanced rehabilitation experiences. The following facets illustrate the key components of state-of-the-art facilities and their impact on the delivery of quality care.
- Advanced Equipment
Cutting-edge technology, such as isokinetic dynamometers, electromyography equipment, and advanced therapeutic modalities, allows practitioners to accurately assess patient progress, deliver targeted interventions, and accelerate recovery. Isokinetic testing, for example, provides objective data on muscle strength and function, allowing for precise exercise prescription and monitoring of rehabilitation progress. Advanced modalities like laser therapy or shockwave therapy offer non-invasive options for pain management and tissue healing, expanding treatment options and improving patient comfort.
- Specialized Environments
Purpose-built spaces designed for specific therapeutic activities, such as aquatic therapy pools, gait training labs, and balance training areas, enhance the effectiveness of interventions. Aquatic therapy, for instance, utilizes the buoyancy of water to reduce stress on joints, allowing patients with mobility limitations to perform exercises that would be difficult or impossible on land. Gait training labs equipped with treadmills, motion capture systems, and force platforms enable precise analysis and retraining of walking patterns, benefiting individuals recovering from stroke, injury, or surgery. These specialized environments facilitate targeted interventions and optimize patient progress.
- Accessibility and Design
Accessibility features within state-of-the-art facilities ensure that individuals with varying levels of physical ability can access and benefit from treatment. Ramps, elevators, accessible restrooms, and adjustable treatment tables accommodate patients with mobility challenges, creating a more inclusive and welcoming environment. Thoughtful design elements, such as well-lit spaces, comfortable waiting areas, and private treatment rooms, enhance patient comfort and promote a positive rehabilitation experience.
- Integration of Technology
The integration of technology within modern facilities enhances communication, data management, and patient engagement. Electronic health records streamline administrative processes, facilitate secure information sharing, and enhance communication between healthcare providers. Telehealth platforms expand access to care, allowing patients in remote areas or with transportation challenges to receive virtual consultations and remote monitoring. Patient portals provide convenient access to appointment scheduling, medical records, and educational resources, empowering patients to actively participate in their care.
These integrated components of state-of-the-art facilities contribute significantly to the overall quality and effectiveness of physical therapy in Roseburg. By providing practitioners with access to advanced tools, specialized environments, and integrated technology, these facilities support the delivery of evidence-based interventions, enhance patient outcomes, and contribute to a more positive and efficient rehabilitation experience. This investment in modern facilities ultimately benefits the community by promoting improved health, well-being, and functional restoration for individuals seeking restorative treatment.
6. Accessible Locations
Convenient access to restorative treatment is crucial for individuals in Roseburg seeking to improve their physical well-being. Geographic accessibility influences an individual’s ability to initiate and maintain consistent engagement with necessary care. Proximity, transportation options, and facility distribution all contribute to the overall accessibility of these services. The following facets explore the components of accessible locations and their impact on rehabilitation within the Roseburg community.
- Proximity to Residential Areas
Locations situated near residential neighborhoods reduce travel time and associated costs, increasing the likelihood of consistent attendance and adherence to treatment plans. Reduced travel burdens benefit individuals with limited mobility, transportation challenges, or time constraints. For example, a clinic located within walking distance of a residential area offers significant advantages for older adults or individuals recovering from surgery who may have difficulty driving or using public transport. This convenience fosters consistent engagement with therapy, promoting better outcomes and reducing the likelihood of treatment interruption due to logistical barriers.
- Transportation Options
The availability of reliable public transportation, accessible parking, and proximity to major roadways impacts an individual’s ability to reach treatment facilities. Adequate transportation infrastructure supports consistent access, reducing the influence of logistical challenges on treatment adherence. For instance, a clinic situated near a bus route expands access for individuals who rely on public transport. Similarly, ample accessible parking accommodates individuals with mobility impairments, ensuring they can safely and conveniently access care. Addressing transportation barriers is essential for ensuring equitable access to rehabilitation services for all members of the community.
- Distribution of Facilities
A strategic distribution of facilities throughout Roseburg ensures equitable access for residents across different neighborhoods and geographic areas. Minimizing travel distances for individuals in various parts of the community reduces disparities in access and promotes utilization of services. For example, having clinics located in both the downtown core and surrounding residential areas ensures that individuals across the city have convenient access to care, regardless of their location. Strategic facility placement minimizes travel burdens, increases convenience, and enhances the likelihood of individuals seeking and completing necessary treatment.
- Facility Accessibility Features
Accessibility features within the facilities themselves, such as ramps, elevators, and accessible restrooms, are crucial for accommodating individuals with mobility impairments. These features ensure that individuals with disabilities can navigate the facility comfortably and participate fully in treatment programs. For example, a clinic with a ramp entrance allows individuals using wheelchairs to access the building independently. Similarly, accessible restrooms and treatment tables accommodate individuals with varying mobility levels, fostering an inclusive environment that supports participation for all individuals seeking rehabilitation services.
Accessible locations are essential for fostering community health and well-being by ensuring individuals can conveniently access necessary rehabilitation services. The strategic placement of facilities, coupled with accessible design features and consideration of transportation options, directly impacts the likelihood of individuals initiating and completing treatment programs, ultimately contributing to better health outcomes within the Roseburg area. These accessibility considerations directly contribute to a more equitable and effective healthcare system by removing barriers to care and promoting consistent engagement in restorative therapies. This emphasis on accessible locations underscores the commitment to providing quality, patient-centered care that empowers individuals to achieve optimal physical function and overall well-being.
7. Patient-Centered Care
Patient-centered care forms a cornerstone of effective rehabilitation within the Roseburg community. This approach prioritizes individual needs, preferences, and values throughout the treatment process. Unlike a standardized approach, patient-centered care recognizes that each individual presents with unique circumstances, requiring tailored interventions and a collaborative approach. This model of care directly influences treatment effectiveness and patient satisfaction. For instance, a practitioner employing patient-centered principles might adapt exercise protocols based on a patient’s expressed discomfort or modify treatment schedules to accommodate work or family obligations. This responsiveness to individual needs fosters a stronger therapeutic alliance, enhances motivation, and ultimately contributes to better outcomes. The integration of patient-centered principles extends beyond simply addressing physical ailments; it encompasses emotional and psychosocial well-being, recognizing the interconnectedness of mind and body within the healing process.
Several key elements characterize patient-centered care within this specific context. Respect for patient autonomy is paramount, ensuring individuals are actively involved in decision-making regarding their treatment plan. Clear and empathetic communication fosters understanding and trust, allowing patients to feel heard and respected. Shared decision-making empowers individuals to actively participate in choosing treatment options that align with their values and preferences. For example, a patient might express a preference for non-invasive treatment options, prompting a discussion with the practitioner regarding alternative approaches. This collaborative process ensures that the chosen interventions align with the patient’s individual circumstances and promote a sense of ownership over the rehabilitation journey. Consider a patient recovering from a stroke; incorporating their personal goals, such as regaining the ability to walk their dog, into the treatment plan enhances motivation and reinforces the purpose behind the therapeutic exercises. This focus on individual aspirations within the context of restorative care reinforces the core principles of patient-centered practice.
Patient-centered care represents a shift from a purely biomedical approach to one that recognizes the individual as a whole person with unique needs and aspirations. This model not only improves treatment adherence and outcomes but also fosters a more positive and empowering rehabilitation experience. By prioritizing individual preferences, values, and active participation, patient-centered care enhances the therapeutic relationship, promotes patient satisfaction, and ultimately contributes to improved health and well-being within the Roseburg community. Challenges may include balancing individualized care with resource constraints, but the benefits of fostering patient autonomy and shared decision-making ultimately contribute to more effective and sustainable healthcare practices.
Frequently Asked Questions
This section addresses common inquiries regarding restorative movement services in Roseburg, Oregon. The information provided aims to clarify potential uncertainties and provide helpful insights for individuals considering these services.
Question 1: What conditions can benefit from restorative movement interventions?
Numerous conditions, including back pain, arthritis, post-surgical rehabilitation, sports injuries, and neurological disorders, can benefit. Treatment aims to improve mobility, reduce pain, and restore function.
Question 2: How does one find a qualified practitioner in Roseburg?
Recommendations from physicians, online directories specializing in healthcare providers, and professional organizations can assist in locating qualified practitioners. Verifying credentials and licensure is essential.
Question 3: What should one expect during an initial consultation?
Initial consultations typically involve a comprehensive assessment of medical history, current condition, and functional limitations. Discussion of goals and potential treatment approaches is standard. A personalized plan may be outlined.
Question 4: How long does a typical treatment session last, and how many sessions might be required?
Session duration and the number of sessions required vary based on individual needs and the nature of the condition. Treatment plans are tailored to address specific goals and may be adjusted based on progress.
Question 5: What is the role of patient participation in the rehabilitation process?
Active patient participation, including adherence to prescribed exercises and open communication with practitioners, is crucial for successful outcomes. Patient commitment contributes significantly to progress and overall effectiveness of treatment.
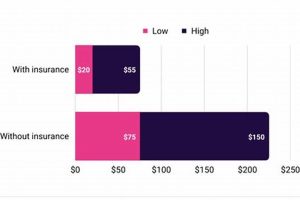
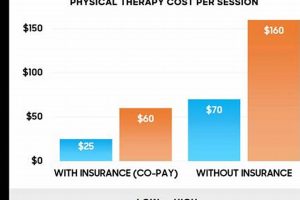
Question 6: Does insurance typically cover these services?
Insurance coverage for restorative movement services varies depending on individual plans and specific conditions. Directly contacting the insurance provider clarifies coverage details and any pre-authorization requirements.
Understanding these key aspects of restorative treatment empowers informed decisions regarding healthcare. Consulting with qualified practitioners provides personalized guidance based on individual needs and circumstances.
The following section delves into the diverse specializations within the field of restorative movement, highlighting the varied expertise available within the Roseburg community.
Physical Therapy Roseburg
This exploration of restorative treatment options within the Roseburg community has highlighted key aspects of accessing and benefiting from these vital services. From the importance of qualified practitioners and individualized treatment plans to the significance of state-of-the-art facilities and accessible locations, the multifaceted nature of effective rehabilitation has been examined. The emphasis on evidence-based techniques and patient-centered care underscores the commitment to providing high-quality, personalized interventions tailored to individual needs and goals. Understanding the comprehensive nature of assessments, the role of patient participation, and the various specializations within the field empowers individuals to make informed decisions regarding their healthcare journey.
Restorative treatment offers a path to improved physical function, pain management, and enhanced well-being within the Roseburg community. Access to these services represents an investment in individual and community health, empowering individuals to regain independence and participate more fully in life’s activities. Seeking timely intervention and engaging actively in the rehabilitation process unlocks the potential for transformative outcomes, fostering a healthier, more vibrant future for individuals and the community as a whole.