The duration of a typical appointment for rehabilitative treatment varies depending on individual needs and the specific treatment plan. Factors influencing appointment length include the type and severity of the condition being addressed, the patient’s overall health, and the specific techniques employed by the therapist. A session focusing on a single, isolated injury might be shorter than one addressing multiple areas or chronic conditions. For instance, a post-surgical rehabilitation appointment might be longer and more intensive than one for a minor strain.
Appropriate appointment durations are crucial for effective rehabilitation. Sufficient time allows for thorough assessment, targeted interventions, and proper patient education. Rushed sessions may compromise treatment efficacy and potentially hinder progress. Historically, the understanding of optimal treatment durations has evolved alongside advancements in therapeutic techniques and a growing body of research demonstrating the importance of individualized care. This evolution underscores the value of consultations with qualified professionals to determine the most suitable treatment plan.
This discussion will further explore the various factors influencing treatment times, including specific types of conditions and therapeutic approaches. Additional topics will include the role of patient engagement in maximizing the benefits of each appointment and strategies for optimizing the rehabilitation process.
Tips for Optimizing Treatment Appointment Time
Maximizing the effectiveness of rehabilitation requires careful consideration of several factors related to appointment duration. The following tips offer guidance for optimizing treatment time and enhancing overall outcomes.
Tip 1: Open Communication with Therapists: Patients are encouraged to discuss scheduling needs and treatment expectations with therapists. Clear communication ensures that appointments are appropriately scheduled to address specific requirements.
Tip 2: Punctuality and Preparation: Arriving on time and adequately prepared for appointments allows therapists to dedicate the full scheduled time to treatment. This includes wearing appropriate attire and completing any pre-appointment instructions.
Tip 3: Active Participation: Active engagement in the treatment process, including asking clarifying questions and following prescribed exercises, contributes to efficient use of appointment time.
Tip 4: Realistic Expectations: Understanding that recovery takes time and that appointment durations are tailored to individual needs helps manage expectations and promotes adherence to the treatment plan.
Tip 5: Consistent Attendance: Regular attendance at scheduled appointments is crucial for maintaining treatment momentum and achieving optimal outcomes. Rescheduling should be minimized whenever possible.
Tip 6: Honest Feedback: Providing therapists with honest feedback regarding pain levels, progress, and any challenges encountered allows for adjustments to the treatment plan and ensures that each session is as productive as possible.
Tip 7: Planning for Potential Delays: Allotting extra time for travel and other potential delays can minimize disruptions and ensure that the full benefit of each appointment is realized.
By adhering to these tips, individuals undergoing rehabilitation can contribute to the efficiency and effectiveness of their treatment appointments, ultimately leading to improved outcomes and a faster return to optimal function.
This understanding of optimizing appointment time contributes to a comprehensive approach to rehabilitation, encompassing not only the duration of sessions but also the active role patients play in maximizing their benefits. The subsequent conclusion will summarize the key takeaways and reinforce the importance of individualized care in achieving successful rehabilitation outcomes.
1. Patient's Condition
A patient’s specific condition plays a pivotal role in determining the duration of physical therapy sessions. The complexity, severity, and stage of the condition directly influence the type and intensity of treatment required, thereby impacting appointment length. Understanding this connection is crucial for establishing realistic expectations and developing effective treatment plans.
- Acute vs. Chronic Conditions:
Acute conditions, such as recent sprains or fractures, may initially require shorter, more frequent sessions focused on pain management and restoring basic function. Chronic conditions, like arthritis or chronic back pain, often necessitate longer sessions incorporating a wider range of therapeutic modalities and exercises aimed at long-term management.
- Severity of the Condition:
A mild ankle sprain might require shorter sessions than a severe ankle fracture requiring extensive rehabilitation. The severity dictates the intensity and duration of treatment needed to achieve functional goals.
- Stage of Healing:
The healing stage significantly impacts session duration. Initial sessions for acute injuries might be shorter and focused on pain control and range of motion. As healing progresses, sessions might lengthen to incorporate strengthening and functional exercises.
- Presence of Comorbidities:
Existing medical conditions, such as diabetes or heart disease, can influence the intensity and duration of physical therapy. These comorbidities may require modified exercises and closer monitoring, potentially impacting session length.
These factors underscore the individualized nature of physical therapy treatment. The interplay between the patient’s condition and session duration highlights the importance of thorough assessments and ongoing communication between the patient and therapist. This ensures that treatment plans are tailored to specific needs and adapted as the condition evolves, ultimately optimizing the rehabilitation process.
2. Treatment Goals
Treatment goals play a crucial role in determining the appropriate duration of physical therapy sessions. Clearly defined objectives, ranging from pain reduction to functional restoration, directly influence the intensity, frequency, and length of each appointment. Understanding this connection is essential for developing effective treatment plans and maximizing patient outcomes.
- Pain Management:
When pain reduction is the primary goal, initial sessions might be shorter and focused on modalities like ice, heat, or electrical stimulation. As pain subsides, sessions might gradually lengthen to incorporate therapeutic exercises and manual therapy techniques aimed at addressing the underlying cause of the pain.
- Restoring Range of Motion:
If limited range of motion is a primary concern, sessions might involve manual therapy, stretching, and joint mobilization techniques. The duration of these sessions depends on the severity of the limitation and the specific joints involved. More restricted joints may require longer sessions to achieve meaningful improvements.
- Improving Strength and Endurance:
Treatment plans focused on building strength and endurance typically involve therapeutic exercises using resistance bands, weights, or bodyweight. These sessions might be longer to accommodate multiple sets and repetitions of various exercises targeting specific muscle groups.
- Regaining Functional Independence:
When the goal is to restore functional independence, such as walking, dressing, or performing daily activities, sessions may involve task-specific training and exercises simulating real-life scenarios. These sessions often require longer durations to allow for practice and adaptation of functional movements.
The interplay between treatment goals and session duration highlights the individualized nature of physical therapy. Establishing clear, measurable goals at the outset of treatment allows therapists to tailor session length and frequency to meet specific patient needs. This approach ensures that each appointment contributes effectively towards achieving desired outcomes and optimizing the overall rehabilitation process.
3. Therapist's Approach
A therapist’s approach significantly influences the duration of physical therapy sessions. Treatment philosophies, preferred techniques, and individual practice styles contribute to variations in appointment length. Understanding these influences provides valuable context for patients navigating the rehabilitation process.
- Manual Therapy Emphasis:
Therapists who prioritize hands-on techniques, such as joint mobilization, soft tissue mobilization, or manual stretching, might require longer sessions to allow adequate time for these individualized treatments. The complexity of the condition and the specific manual therapy approach employed contribute to variations in session duration.
- Exercise-Based Approach:
Therapists emphasizing therapeutic exercise might allocate more session time to instructing, guiding, and supervising patients through prescribed movements. The complexity and number of exercises influence the overall appointment length. Sufficient time ensures proper form and technique, maximizing exercise benefits and minimizing the risk of re-injury.
- Technology Integration:
The integration of technology, such as ultrasound, electrical stimulation, or laser therapy, can influence session duration. While some modalities can be administered concurrently with other treatments, others require dedicated time, potentially lengthening the appointment. The specific technology utilized and its integration into the overall treatment plan impacts session length.
- Patient Education Focus:
Therapists who prioritize patient education might dedicate more time to explaining the condition, demonstrating exercises, and providing self-management strategies. This comprehensive approach, though potentially lengthening individual sessions, empowers patients with knowledge and tools for long-term self-care.
Practical implications of varying therapeutic approaches extend beyond session duration. A therapist’s chosen methodology impacts the overall treatment plan, influencing the frequency and total number of sessions required to achieve desired outcomes. For example, a manual therapy-focused approach might require fewer but longer sessions compared to an exercise-based approach. Understanding these nuances allows patients to make informed decisions about their rehabilitation journey.
In summary, the therapist’s approach plays a critical role in determining session duration and overall treatment structure. Recognizing the interplay between therapeutic philosophies, preferred techniques, and individual practice styles empowers patients to engage actively in their rehabilitation and fosters a collaborative relationship with their therapist. This collaborative approach is essential for optimizing treatment outcomes and achieving long-term functional goals.
4. Clinic Policies
Clinic policies exert a significant influence on the duration of physical therapy sessions. These policies, designed to manage scheduling, resource allocation, and billing practices, directly impact appointment lengths and overall treatment structure. Understanding this connection is crucial for both patients and therapists navigating the rehabilitation landscape.
Several factors within clinic policies contribute to variations in session duration. Scheduling practices, often dictated by staffing levels and patient volume, can influence appointment availability and length. Clinics operating with limited staff or high patient demand may offer shorter appointment slots to accommodate more individuals. Conversely, clinics with greater staffing flexibility might offer longer appointments, allowing for more comprehensive treatment within a single session. Resource allocation, including the availability of treatment equipment and space, also impacts session duration. Limited access to specialized equipment might necessitate shorter, more focused appointments to ensure equitable access for all patients. Billing practices, particularly those involving insurance companies, can influence appointment length. Some insurance providers might impose restrictions on session duration or require pre-authorization for longer appointments, impacting the structure of the treatment plan. For instance, a clinic might schedule shorter, more frequent sessions to comply with insurance guidelines, even if longer sessions might be clinically beneficial.
The practical implications of these policies extend beyond individual appointment lengths. Clinic scheduling practices influence the overall frequency and spacing of appointments, impacting the continuity of care. Resource allocation can affect the types of treatments offered and the therapist’s ability to integrate diverse therapeutic modalities. Billing practices, driven by insurance contracts and regulations, can impact patient access to specific treatments and the overall affordability of care. Understanding the interplay between these factors allows patients to navigate scheduling challenges and make informed decisions about their treatment options. For therapists, awareness of clinic policies is essential for effective treatment planning and patient advocacy. Navigating these policies requires clear communication between patients, therapists, and administrative staff, ensuring that treatment plans align with individual needs while adhering to clinic guidelines. This collaborative approach optimizes the rehabilitation experience within the framework of existing policy constraints.
5. Thirty to Sixty Minutes (Typical)
The typical duration of a physical therapy session, often falling within the 30- to 60-minute range, represents a practical benchmark for scheduling and resource allocation. This timeframe allows for a balanced approach, incorporating assessment, treatment, and patient education within a manageable period. Several factors contribute to this established norm. Shorter durations may not provide adequate time for thorough evaluations or effective interventions, potentially compromising treatment efficacy. Conversely, excessively long sessions can lead to patient fatigue and decreased engagement, hindering progress. The 30- to 60-minute window allows therapists to deliver focused interventions while respecting patient limitations and optimizing engagement. For instance, a 45-minute session might involve 15 minutes of assessment and manual therapy, followed by 20 minutes of therapeutic exercise and 10 minutes of patient education and home exercise instruction. This structured approach ensures that each session component receives appropriate attention.
Practical implications of this typical duration extend to various aspects of rehabilitation. Scheduling efficiency improves as clinics can allocate standardized appointment slots, optimizing patient flow and therapist availability. Cost-effectiveness is enhanced as treatment plans can be structured around predictable session durations, facilitating insurance reimbursement and patient budgeting. Patient adherence improves when sessions are manageable in length, reducing the burden of time commitment and promoting consistent attendance. However, deviations from this typical range are common and often necessary. Complex cases, such as post-surgical rehabilitation or neurological conditions, might require longer sessions to address multifaceted needs. Pediatric or geriatric populations might benefit from shorter, more frequent sessions to accommodate reduced attention spans or physical limitations. These adjustments highlight the individualized nature of physical therapy and the importance of tailoring treatment plans to specific patient characteristics and goals.
In summary, the 30- to 60-minute timeframe for physical therapy sessions represents a practical guideline, balancing treatment needs with scheduling efficiency and patient tolerance. While this benchmark provides a valuable framework, deviations are often necessary to address individual circumstances and optimize rehabilitation outcomes. Recognizing this balance between standardized practice and individualized care is crucial for effective treatment planning and patient-centered rehabilitation.
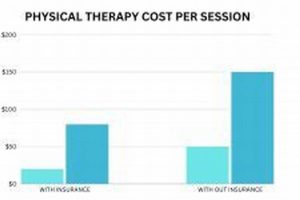
6. Insurance Coverage
Insurance coverage plays a significant role in determining the duration and frequency of physical therapy sessions. Policies vary widely, influencing access to care and shaping the structure of treatment plans. Understanding the interplay between insurance benefits and rehabilitation is crucial for both patients and providers.
- Pre-authorization Requirements:
Many insurance policies require pre-authorization for physical therapy services, especially for extended treatment plans. This process involves submitting a treatment plan to the insurance company for approval before initiating therapy. Pre-authorization requirements can influence session duration, as insurers may only approve a specific number of visits or a limited timeframe for treatment. For example, an insurer might authorize 12 sessions over six weeks, influencing the scheduling and intensity of each appointment.
- Visit Limits:
Some insurance plans impose limits on the number of physical therapy visits allowed within a specific timeframe, such as a year or benefit period. These limitations can directly impact session duration, as therapists may need to condense treatment plans or prioritize specific interventions to maximize outcomes within the allotted visits. For instance, if a patient has a limit of 20 visits per year, therapists might opt for longer sessions to address multiple treatment goals concurrently, potentially impacting scheduling flexibility.
- Coverage for Specific Modalities:
Insurance coverage for specific modalities, such as manual therapy, dry needling, or aquatic therapy, varies considerably. Some plans may cover these interventions fully, while others offer partial reimbursement or exclude them altogether. This variation can influence session length and treatment approach. For instance, if a patient’s insurance does not cover aquatic therapy, a land-based alternative might require longer sessions to achieve similar outcomes.
- Network Requirements:
Many insurance plans require patients to seek care from in-network providers to receive maximum benefits. Out-of-network services often incur higher out-of-pocket costs or may not be covered at all. This restriction can limit patient choice and potentially influence session duration if in-network providers have different scheduling practices or treatment approaches compared to preferred out-of-network options. A patient might need to accept shorter session durations with an in-network provider due to financial constraints.
These facets of insurance coverage interact in complex ways, shaping the parameters of physical therapy treatment. Negotiating these complexities requires open communication between patients, therapists, and insurance providers. Understanding policy limitations and exploring available options empowers patients to advocate for their rehabilitation needs and make informed decisions about their care. This collaborative approach, informed by the realities of insurance coverage, is essential for maximizing treatment efficacy and achieving optimal functional outcomes within the existing healthcare landscape.
Frequently Asked Questions
This section addresses common inquiries regarding the duration of rehabilitative treatment appointments. Clear understanding of these aspects is crucial for effective treatment planning and successful outcomes.
Question 1: How does the nature of an injury influence appointment length?
The complexity and severity of the condition being addressed directly impact session duration. Conditions requiring extensive rehabilitation or specialized techniques typically necessitate longer appointments.
Question 2: Are all appointments the same length throughout a treatment plan?
Appointment duration may vary throughout a treatment plan. Initial sessions might be shorter, focusing on assessment and pain management, while later sessions might lengthen to incorporate more complex exercises and functional training.
Question 3: What role does insurance coverage play in determining session length?
Insurance policies often influence session duration. Coverage limitations or pre-authorization requirements might necessitate shorter, more frequent appointments, even if longer sessions would be clinically ideal.
Question 4: Can patients request longer or shorter appointments based on personal preferences?
While patient preferences are considered, appointment durations are primarily determined by clinical need and treatment goals. Open communication between patients and therapists ensures that sessions are appropriately tailored to individual requirements while adhering to established guidelines.
Question 5: How does a therapist’s specialization influence appointment length?
A therapist’s specialization and preferred treatment techniques can influence session duration. Therapists specializing in manual therapy, for example, might require longer appointments than those focusing primarily on exercise-based interventions.
Question 6: What can one do to ensure appointments are used effectively?
Arriving on time, wearing appropriate attire, and actively engaging in prescribed activities maximize the benefits of each session. Open communication with the therapist regarding progress and any challenges encountered ensures that treatment plans remain aligned with individual needs.
Understanding these aspects of appointment duration contributes significantly to a successful rehabilitation experience. Open communication and collaborative decision-making between patients and therapists remain crucial for optimizing treatment outcomes.
The following section will provide concluding insights into the importance of individualized care in achieving optimal rehabilitation results.
Conclusion
Exploration of physical therapy session duration reveals a complex interplay of factors influencing appointment length. Individual patient needs, specific conditions, treatment goals, therapist approaches, clinic policies, and insurance coverage all contribute to variations in session times. While the typical 30- to 60-minute benchmark provides a general framework, deviations are common and often necessary to accommodate individual circumstances and optimize treatment outcomes. Effective communication between patients and therapists is paramount in determining appropriate session durations aligned with individual rehabilitation goals.
Optimizing physical therapy outcomes requires a comprehensive understanding of the factors influencing session duration. Recognizing the individualized nature of rehabilitation and engaging in collaborative decision-making with qualified professionals empowers individuals to navigate the complexities of treatment planning and maximize the benefits of each appointment. Further research into the efficacy of varying session durations for specific conditions promises to refine treatment approaches and enhance rehabilitation outcomes in the future. This ongoing evolution of knowledge underscores the dynamic nature of physical therapy and its commitment to individualized, patient-centered care.