Restorative treatment provided in locally-based healthcare facilities often involves individualized programs designed to improve mobility, manage pain, and restore function after illness, injury, or surgery. These programs may include therapeutic exercises, manual therapy techniques, and modalities such as heat, cold, and electrical stimulation. A typical example might involve a patient recovering from a knee replacement undergoing a tailored exercise regimen to regain strength and range of motion.
Access to rehabilitative services in a familiar setting offers distinct advantages. It allows patients to receive care close to home, minimizing travel time and disruption to daily routines. This proximity also facilitates stronger connections with therapists and fosters a supportive environment conducive to healing. Historically, the evolution of these localized services reflects a growing emphasis on patient-centered care and the recognition of rehabilitation’s vital role in overall health and well-being. Such localized care contributes significantly to improved patient outcomes and reduced healthcare costs by preventing re-hospitalizations and promoting faster returns to normal activity.
This article will further explore key aspects of rehabilitation within local healthcare settings, including specific treatment approaches, the role of interdisciplinary teams, and the impact of technological advancements on patient care.
Tips for Maximizing Recovery through Rehabilitation in Local Healthcare Settings
Optimizing the benefits of restorative treatment requires active patient participation and a clear understanding of the recovery process. The following tips provide valuable guidance for individuals undergoing rehabilitation.
Tip 1: Communicate Openly with Therapists: Clear communication regarding pain levels, limitations, and goals is crucial for developing a personalized treatment plan. Detailed feedback allows therapists to adjust exercises and techniques as needed.
Tip 2: Adhere to the Prescribed Program: Consistent attendance at therapy sessions and diligent completion of home exercises are essential for progress. Following the prescribed program maximizes the likelihood of achieving optimal functional outcomes.
Tip 3: Set Realistic Goals: Recovery takes time and effort. Setting achievable milestones helps maintain motivation and prevents discouragement. Working collaboratively with therapists to establish realistic expectations ensures a positive experience.
Tip 4: Prioritize Rest and Recovery: Adequate rest allows the body to heal and rebuild strength. Balancing therapeutic activities with periods of rest is vital for avoiding overexertion and preventing setbacks.
Tip 5: Maintain a Healthy Lifestyle: Proper nutrition, hydration, and stress management contribute significantly to the healing process. Adopting healthy habits supports overall well-being and enhances the effectiveness of therapy.
Tip 6: Seek Support When Needed: Connecting with family, friends, or support groups can provide emotional and practical assistance during recovery. A strong support system fosters resilience and encourages adherence to the treatment plan.
Tip 7: Ask Questions: Do not hesitate to inquire about any aspect of the rehabilitation process. Understanding the rationale behind specific treatments and exercises empowers patients and promotes active participation.
By following these guidelines, individuals can actively participate in their rehabilitation journey and maximize their potential for a successful recovery. These proactive steps empower patients to regain function, manage pain effectively, and improve their overall quality of life.
The following section will discuss resources and support services available to individuals undergoing rehabilitation in local healthcare settings.
1. Localized Care
Localized care forms a cornerstone of community hospital physical therapy, emphasizing the provision of essential rehabilitative services within the patient’s own community. This approach recognizes the significant impact proximity plays in patient outcomes, adherence to treatment plans, and overall well-being. By reducing geographical barriers, localized care enhances accessibility and fosters a stronger therapeutic relationship between patients and providers.
- Reduced Travel Burden
Minimizing travel time and associated expenses alleviates a significant burden for patients, particularly those with mobility limitations or residing in rural areas. This convenience allows individuals to focus on their recovery rather than logistical challenges, promoting consistent attendance at therapy sessions and improved adherence to prescribed home exercise programs.
- Enhanced Patient Comfort and Familiarity
Receiving care in a familiar environment, often close to family and friends, contributes to a sense of comfort and security. This familiarity can reduce anxiety and stress associated with medical treatment, fostering a more positive and productive therapeutic experience.
- Strengthened Community Integration
Localized care facilitates seamless integration back into the community following rehabilitation. Patients can readily apply newly acquired skills and strategies within their familiar surroundings, promoting independence and long-term success in managing their condition.
- Increased Accessibility to Support Systems
Proximity to family and local support networks provides patients with essential emotional and practical assistance during recovery. This support network plays a crucial role in encouraging adherence to treatment plans and promoting overall well-being.
These facets of localized care underscore its vital role in the effectiveness of community hospital physical therapy. By addressing geographical, emotional, and social factors, localized care optimizes the rehabilitation process, leading to improved patient outcomes, increased patient satisfaction, and enhanced community health.
2. Personalized Treatment
Personalized treatment plans represent a critical component of effective rehabilitation within community hospital settings. Recognizing that each individual presents with unique needs, limitations, and goals, therapists develop tailored programs designed to optimize functional outcomes and enhance the recovery process. This individualized approach considers factors such as age, medical history, injury specifics, lifestyle, and personal preferences. The connection between personalized treatment and community hospital physical therapy lies in the ability to deliver highly specific care within a convenient and accessible setting.
For example, a patient recovering from a stroke may require a treatment plan focusing on regaining upper extremity function and improving balance, while a patient rehabilitating from a knee injury may prioritize restoring range of motion and strengthening surrounding musculature. Tailoring interventions to address these distinct needs optimizes recovery and facilitates a return to prior levels of activity. The community hospital setting allows for this personalized care to be delivered close to home, reducing travel burdens and increasing adherence to therapy schedules. Moreover, the smaller scale and community focus of these hospitals often foster stronger patient-therapist relationships, further enhancing the personalization of care.
This understanding of the crucial link between personalized treatment and community hospital physical therapy underscores the value of these local facilities in providing high-quality, patient-centered rehabilitation services. Addressing individual needs through tailored interventions within accessible settings leads to improved patient outcomes, increased patient satisfaction, and enhanced community health. Challenges remain in ensuring equitable access to these personalized services, particularly for individuals in underserved communities. Continued efforts to address disparities and promote equitable access will be vital to maximizing the benefits of personalized treatment within community hospital settings.
3. Restoring Function
Restoring functional independence represents a central objective of physical therapy within community hospital settings. Rehabilitation programs focus on helping individuals regain the ability to perform essential daily tasks, fostering greater autonomy and improving overall quality of life. This emphasis on functional restoration aligns with the community hospital’s mission of providing patient-centered care that addresses individual needs within a familiar and supportive environment.
- Activities of Daily Living (ADLs)
Therapeutic interventions often target basic self-care activities such as dressing, bathing, grooming, and eating. Regaining independence in these areas allows individuals to manage personal care without assistance, promoting self-sufficiency and reducing reliance on caregivers.
- Instrumental Activities of Daily Living (IADLs)
Beyond basic self-care, rehabilitation programs also address more complex activities essential for independent living. These may include meal preparation, medication management, household chores, and community mobility. Restoring competence in IADLs empowers individuals to participate more fully in their daily routines and maintain an active role within the community.
- Mobility and Ambulation
Restoring mobility and safe ambulation are critical components of functional restoration. Therapeutic exercises and gait training improve strength, balance, and coordination, enabling individuals to navigate their environment with greater confidence and reducing the risk of falls.
- Work-Related Activities
For individuals whose functional limitations impact their ability to work, rehabilitation programs may incorporate job-specific tasks and simulations. This targeted approach facilitates a successful return to work, promoting financial independence and social engagement.
By prioritizing functional restoration, community hospital physical therapy programs play a vital role in empowering individuals to regain independence, reintegrate into the community, and achieve a higher quality of life. This emphasis on functional outcomes underscores the value of community-based rehabilitation services in promoting individual well-being and fostering healthier communities. The accessibility and personalized care provided within these settings contribute significantly to successful functional recovery and improved long-term outcomes.
4. Managing Pain
Effective pain management constitutes a cornerstone of community hospital physical therapy, significantly impacting patient comfort, functional recovery, and overall well-being. Addressing pain allows individuals to engage more fully in therapeutic exercises and activities, maximizing the benefits of rehabilitation and facilitating a return to daily routines. This focus on pain management within community settings underscores the holistic approach to patient care, recognizing the interconnectedness of physical, emotional, and social well-being.
- Manual Therapy Techniques
Hands-on techniques, such as soft tissue mobilization, joint mobilization, and manual traction, address musculoskeletal imbalances and reduce pain. For example, a therapist might use soft tissue mobilization to release muscle tension in a patient’s neck, alleviating pain and improving range of motion. Within the community hospital setting, these manual therapy techniques are readily integrated into personalized treatment plans, providing targeted pain relief and facilitating functional recovery.
- Therapeutic Modalities
Modalities like heat, cold, ultrasound, and electrical stimulation offer non-invasive approaches to pain management. Heat therapy can reduce muscle stiffness and pain, while cold therapy can decrease inflammation and swelling after an acute injury. A community hospital therapist might use ultrasound to promote tissue healing and reduce pain in a patient with tendinitis. The availability of these modalities within the community setting expands treatment options and enhances pain management strategies.
- Therapeutic Exercise
Targeted exercise programs play a crucial role in reducing pain, improving strength and flexibility, and restoring function. For example, a patient with low back pain might benefit from a core strengthening program to improve stability and reduce pain. Community hospital physical therapists design individualized exercise programs to address specific needs and functional limitations, enhancing pain management and promoting long-term recovery.
- Patient Education
Empowering patients with knowledge about their condition and pain management strategies is essential. Education may include instruction on proper body mechanics, pain-relieving postures, and self-management techniques. Within the community hospital environment, therapists provide personalized education and support, fostering self-efficacy and promoting active participation in the pain management process.
These integrated pain management strategies within community hospital physical therapy demonstrate a commitment to comprehensive patient care. Addressing pain not only improves patient comfort but also facilitates active participation in rehabilitation, leading to improved functional outcomes, enhanced quality of life, and successful reintegration into the community. The accessibility and personalized care characteristic of community hospital settings enhance the effectiveness of these pain management strategies, fostering a positive patient experience and promoting overall well-being.
5. Improving Mobility
Enhanced mobility forms a cornerstone of successful rehabilitation within community hospital physical therapy settings. Restoring the ability to move freely and easily is essential for regaining independence, participating in daily activities, and improving overall quality of life. Therapeutic interventions address various aspects of mobility, from basic ambulation to more complex movements required for community engagement and participation in social roles.
- Gait Training
Gait training focuses on improving walking patterns, addressing issues such as stride length, balance, and coordination. A therapist might use assistive devices like walkers or canes initially and progressively challenge the patient to walk independently as they improve. Within the community hospital setting, gait training often occurs in environments that simulate real-world scenarios, preparing patients for navigating various terrains and obstacles encountered in daily life. This focus on practical application enhances the effectiveness of gait training and facilitates a smoother transition back into the community.
- Range of Motion Exercises
Restoring joint range of motion is crucial for performing everyday tasks, such as reaching, bending, and dressing. Therapists guide patients through specific exercises designed to increase flexibility and mobility in affected joints. For instance, a patient recovering from shoulder surgery might engage in exercises to improve shoulder flexion, extension, and rotation. The personalized nature of care within community hospital settings ensures that these exercises are tailored to individual needs and functional goals, optimizing the restoration of range of motion and improving overall mobility.
- Strengthening Exercises
Building strength in weakened muscles is essential for supporting improved mobility and preventing future injuries. Therapists prescribe exercises using body weight, resistance bands, or weights to target specific muscle groups. For example, a patient recovering from a knee injury might engage in quadriceps and hamstring strengthening exercises to improve stability and support ambulation. Community hospital physical therapy programs often incorporate access to exercise equipment and personalized guidance, creating a supportive environment for progressive strengthening and improved mobility.
- Balance and Coordination Training
Improving balance and coordination is vital for preventing falls and maintaining safe mobility. Therapeutic activities might include balance exercises on unstable surfaces or activities that challenge coordination, such as reaching and grasping. For instance, a patient with a neurological condition might benefit from balance training using a balance board or specialized exercise equipment. The availability of these resources within community hospital settings enhances the effectiveness of balance and coordination training, promoting safer mobility and reducing the risk of falls.
These interconnected components of mobility improvement within community hospital physical therapy demonstrate a holistic approach to rehabilitation. By addressing gait, range of motion, strength, and balance, therapists empower patients to regain functional independence, participate more fully in their communities, and achieve a higher quality of life. The accessibility, personalized care, and community-focused approach characteristic of these settings contribute significantly to the effectiveness of mobility interventions and promote successful long-term outcomes.
6. Community Integration
Community integration represents a crucial outcome and integral component of community hospital physical therapy. Successful rehabilitation extends beyond restoring physical function; it empowers individuals to re-engage with their communities and resume meaningful social roles. This reintegration process hinges on the ability to perform activities essential for community participation, such as navigating public transportation, accessing community resources, and engaging in social activities. Community hospital physical therapy programs facilitate this process by providing localized care, personalized treatment plans, and a focus on functional restoration tailored to the individual’s community environment. This connection between community integration and community hospital physical therapy fosters a sense of belonging, reduces social isolation, and promotes overall well-being.
For instance, a patient recovering from a hip replacement might participate in therapy sessions that simulate grocery shopping or navigating public transportation. This practical application of therapeutic exercises within a community context prepares the individual for real-world challenges and fosters greater confidence in their ability to navigate their community independently. Similarly, a patient rehabilitating from a stroke might engage in group therapy sessions that incorporate community outings, promoting social interaction and facilitating reintegration into social networks. These examples illustrate how community hospital physical therapy programs actively promote community integration as a core element of the rehabilitation process. The convenient location of these facilities within the community further enhances reintegration efforts by allowing patients to practice newly acquired skills within their familiar surroundings. This localized approach fosters a sense of continuity and reduces the anxiety associated with transitioning back into community life.
Understanding the vital link between community integration and community hospital physical therapy underscores the importance of adopting a holistic approach to rehabilitation. Addressing physical limitations in isolation is insufficient for achieving optimal patient outcomes. Successful reintegration requires a focus on functional restoration within the context of the individual’s community environment. Community hospital physical therapy programs, by virtue of their location, personalized care, and emphasis on functional restoration, play a pivotal role in facilitating community integration and enhancing the overall well-being of individuals recovering from illness or injury. Challenges remain in ensuring equitable access to these community-based services, particularly for individuals in underserved or geographically isolated communities. Addressing these disparities through targeted outreach and resource allocation is essential for maximizing the benefits of community hospital physical therapy and promoting successful community integration for all individuals.
Frequently Asked Questions
This section addresses common inquiries regarding restorative treatment provided in local healthcare facilities.
Question 1: What types of conditions benefit from therapy in local healthcare settings?
Numerous conditions, including orthopedic injuries, neurological conditions, chronic pain, and post-surgical rehabilitation, can benefit from this type of therapy. Specific programs are tailored to individual needs and may address mobility impairments, pain management, and functional restoration.
Question 2: How does one access these services?
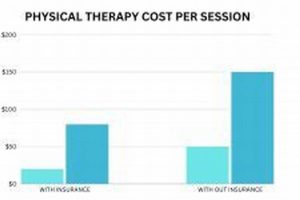
Referrals from physicians or other healthcare providers are often required. Direct access to physical therapy may also be available depending on local regulations and insurance coverage. Contacting local healthcare facilities or insurance providers can provide further guidance on access procedures.
Question 3: What should one expect during an initial evaluation?
Initial evaluations typically involve a comprehensive assessment of the individual’s medical history, current condition, and functional limitations. Therapists conduct physical examinations and assess range of motion, strength, balance, and coordination. This information informs the development of a personalized treatment plan.
Question 4: What is the typical duration of a treatment program?
Treatment duration varies depending on individual needs and the nature of the condition being addressed. Some individuals may require a few weeks of therapy, while others may benefit from longer-term programs. Regular reassessments help determine the appropriate duration and adjust treatment plans as needed.
Question 5: What is the role of the patient in the rehabilitation process?
Active patient participation is crucial for successful rehabilitation. Open communication with therapists, consistent attendance at therapy sessions, and adherence to prescribed home exercise programs contribute significantly to positive outcomes. Patients are encouraged to actively engage in the process and communicate any concerns or questions to their therapists.
Question 6: How can one ensure the quality of these services?
Accreditation by recognized organizations, such as The Joint Commission, signifies a commitment to quality and patient safety. Inquiring about therapist credentials and experience can also provide valuable insights. Reviews and testimonials from other patients may offer additional perspectives on the quality of care provided.
Understanding these key aspects of restorative treatment in local healthcare facilities empowers individuals to make informed decisions and optimize their rehabilitation journey. Access to quality rehabilitative care plays a vital role in improving functional outcomes, enhancing quality of life, and fostering healthier communities.
The following section will delve into specific therapeutic interventions and treatment modalities commonly employed in community hospital physical therapy settings.
Community Hospital Physical Therapy
This exploration of community hospital physical therapy has highlighted its multifaceted role in restoring function, managing pain, and improving mobility for individuals within their local communities. Accessibility, personalized care, and a focus on functional restoration within familiar environments distinguish this approach. From gait training and therapeutic exercises to manual therapy techniques and patient education, the comprehensive nature of these services empowers individuals to regain independence and reintegrate into their communities.
The continued development and support of community hospital physical therapy programs are essential for promoting individual well-being and fostering healthier communities. Investment in these localized services represents an investment in the health and resilience of the population. As healthcare evolves, community-based rehabilitation will play an increasingly vital role in ensuring access to high-quality, patient-centered care that addresses the diverse needs of individuals across the lifespan.