Posterior Leaf of Oblique Fibular Ligament (plof) injuries often occur in conjunction with ankle sprains and can contribute to ongoing instability and pain if left untreated. A specialized rehabilitation program focuses on restoring strength, stability, and function to the injured area. This might include targeted exercises, manual therapy techniques, and modalities like ultrasound or electrical stimulation. For instance, exercises might involve strengthening the peroneal muscles that support the outer ankle or proprioceptive training to improve balance and joint position awareness.
Addressing these specific ligament injuries through focused rehabilitation is vital for preventing chronic ankle instability, reducing pain and swelling, and improving overall lower extremity function. Neglecting this specific ligament can lead to recurrent ankle sprains and long-term issues. Historically, plof injuries were often overlooked or misdiagnosed, contributing to persistent ankle problems. Greater understanding of ankle biomechanics and improved diagnostic techniques have highlighted the significance of this structure in maintaining ankle stability.
This article will further explore the anatomy of the affected ligament, common mechanisms of injury, diagnostic procedures, and various treatment options available, including surgical and non-surgical approaches.
Tips for Managing Posterior Leaf of Oblique Fibular Ligament Injuries
Effective management of these injuries involves a multifaceted approach focusing on pain reduction, restoration of stability, and prevention of recurrence. The following tips offer guidance for navigating recovery.
Tip 1: Seek Professional Assessment: Accurate diagnosis is crucial. Consult a qualified healthcare professional, such as a physician or physical therapist, specializing in ankle injuries for a thorough evaluation and personalized treatment plan.
Tip 2: Control Initial Swelling and Pain: Implement the RICE protocol (Rest, Ice, Compression, Elevation) immediately following injury to minimize swelling and alleviate pain.
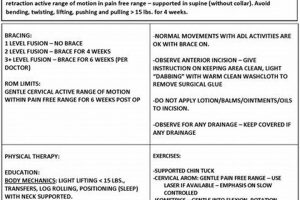
Tip 3: Adhere to Prescribed Rehabilitation: Consistent adherence to the prescribed rehabilitation program is essential for optimal recovery. This includes diligently performing exercises and attending scheduled therapy sessions.
Tip 4: Prioritize Proper Footwear: Supportive footwear is crucial during recovery. Avoid high heels or shoes that lack adequate ankle support. Consider using ankle braces or orthotics as recommended by a healthcare professional.
Tip 5: Gradual Return to Activity: Avoid rushing the return to pre-injury activity levels. Gradually increase activity as tolerated, guided by professional advice, to minimize the risk of re-injury.
Tip 6: Focus on Balance and Proprioception: Incorporate balance and proprioceptive exercises into the rehabilitation program. These exercises improve joint position awareness and stability, reducing the risk of future ankle sprains.
Tip 7: Listen to Your Body: Pay attention to pain signals. Avoid pushing through pain, which could exacerbate the injury. Modify or discontinue activities that cause discomfort and consult with a healthcare professional.
Following these tips can significantly contribute to successful rehabilitation, allowing individuals to regain ankle stability, reduce pain, and return to their desired activity levels. Careful management of these injuries is crucial for preventing long-term complications and maintaining optimal ankle function.
In conclusion, understanding the specific nature of these injuries and following appropriate management strategies is vital for a positive outcome.
1. Diagnosis
Accurate diagnosis forms the cornerstone of effective treatment for Posterior Leaf of the Oblique Fibular Ligament (plof) injuries. Given the subtle nature of these injuries and their frequent association with other ankle ligament sprains, a comprehensive evaluation is essential. The diagnostic process typically involves a thorough clinical examination, including assessment of tenderness, swelling, range of motion, and ligament stability. Specific tests, such as the talar tilt test and anterior drawer test, can help isolate the plof and differentiate it from injuries to the anterior talofibular ligament or calcaneofibular ligament. For example, localized pain along the course of the plof, combined with instability during specific maneuvers, may suggest a plof tear. Diagnostic imaging, such as MRI or ultrasound, may be employed to confirm the diagnosis and assess the extent of the injury, particularly when differentiating between partial and complete tears. A precise diagnosis allows for targeted treatment strategies and informs prognosis.
The importance of accurate diagnosis in plof injuries cannot be overstated. Misdiagnosis or delayed diagnosis can lead to inadequate treatment, resulting in chronic ankle instability, persistent pain, and decreased functional capacity. For instance, if a plof injury is misdiagnosed as a simple ankle sprain and only treated with basic rest and ice, the instability may persist, leading to further complications and delayed recovery. Conversely, a timely and accurate diagnosis allows for prompt initiation of appropriate interventions, including tailored rehabilitation programs, bracing, or surgical intervention when necessary. This proactive approach minimizes the risk of long-term sequelae and facilitates a more efficient return to pre-injury activity levels.
In summary, a comprehensive diagnostic approach is paramount in managing plof injuries. Integrating clinical examination findings with advanced imaging techniques ensures accurate identification and assessment of injury severity. This foundation allows clinicians to develop individualized treatment plans, optimizing patient outcomes and promoting a swift and successful recovery. Challenges remain in differentiating isolated plof injuries from combined ligamentous injuries, highlighting the need for ongoing research and refinement of diagnostic techniques. Ultimately, the precision of the diagnosis directly influences the effectiveness of subsequent plof physical therapy interventions.
2. Pain Management
Pain management constitutes a critical component of rehabilitation following Posterior Leaf of the Oblique Fibular Ligament (plof) injuries. Pain following these injuries arises from tissue damage, inflammation, and potential impingement of surrounding structures. Effective pain management facilitates early mobilization, a cornerstone of successful rehabilitation. Untreated pain hinders active participation in therapeutic exercises, delaying recovery and increasing the risk of chronic pain syndromes. For instance, an individual experiencing significant pain may limit ankle movement, leading to stiffness and decreased range of motion. This, in turn, impairs functional activities such as walking or stair climbing. By effectively managing pain, individuals can engage more fully in rehabilitation, optimizing outcomes. Various pain management strategies can be employed, including pharmacological and non-pharmacological approaches. Pharmacological interventions, such as non-steroidal anti-inflammatory drugs (NSAIDs), can reduce pain and inflammation. Non-pharmacological modalities, such as cryotherapy (ice), compression, elevation, and electrotherapeutic modalities like transcutaneous electrical nerve stimulation (TENS), provide analgesic effects and promote tissue healing. The choice of pain management strategy should be individualized based on the severity of pain, patient preferences, and any coexisting medical conditions.
Beyond immediate pain relief, effective pain management strategies enable earlier initiation of range-of-motion exercises and strengthening programs. These exercises are essential for restoring ankle stability and function, reducing the likelihood of long-term complications such as chronic ankle instability. For example, individuals able to participate in early mobilization exercises due to effective pain control regain range of motion more quickly and experience less muscle atrophy, ultimately facilitating a faster return to pre-injury activity levels. Furthermore, addressing pain early in the rehabilitation process can prevent the development of central sensitization, a phenomenon where the nervous system becomes more sensitive to pain signals, potentially leading to chronic pain even after tissue healing. Therefore, a proactive approach to pain management not only improves patient comfort but also plays a crucial role in preventing long-term disability.
In summary, effective pain management is integral to successful plof physical therapy. By addressing pain early and comprehensively, clinicians create an environment conducive to active patient participation in rehabilitation. This, in turn, promotes optimal restoration of ankle function, reduces the risk of chronic pain and instability, and facilitates a timely return to normal activities. Challenges remain in balancing the need for pain relief with the potential side effects of pharmacological interventions. Further research exploring optimal pain management strategies for plof injuries will continue to refine treatment approaches and improve patient outcomes.
3. Range of Motion
Restoring optimal range of motion constitutes a fundamental objective in posterior leaf of the oblique fibular ligament (plof) physical therapy. Following a plof injury, limitations in ankle range of motion can arise from several factors, including pain, swelling, scar tissue formation, and protective muscle guarding. Restricted dorsiflexion (bringing the foot upwards) and plantarflexion (pointing the foot downwards) can significantly impair functional mobility, affecting activities such as walking, stair climbing, and running. For instance, limited dorsiflexion can lead to a shortened stride length and compensatory gait patterns, increasing the risk of falls and other lower extremity injuries. Therefore, addressing range of motion limitations is crucial for restoring normal biomechanics and preventing long-term functional deficits.
Range of motion exercises play a vital role throughout the rehabilitation process. Early mobilization, within pain tolerance, helps prevent stiffness and promotes tissue healing. Gentle, passive range of motion exercises, often assisted by the therapist, initiate movement and reduce scar tissue adhesion. As pain subsides, active range of motion exercises, performed independently by the individual, progressively increase joint mobility and strengthen surrounding musculature. For example, exercises such as ankle pumps, alphabet tracing with the foot, and towel stretches can target specific movements and improve flexibility. Furthermore, manual therapy techniques, such as joint mobilizations performed by the therapist, can address specific joint restrictions and improve overall ankle mobility. The progression of range of motion exercises should be individualized based on the severity of the injury, tissue healing, and individual patient response.
In conclusion, restoring full, pain-free ankle range of motion is essential for successful plof physical therapy outcomes. Early mobilization, combined with progressive active and passive range of motion exercises and manual therapy techniques, facilitates optimal tissue healing and prevents long-term functional limitations. Challenges remain in balancing the need for early mobilization with the risk of exacerbating pain and inflammation. Further research investigating optimal range of motion protocols for plof injuries will enhance rehabilitation strategies and improve patient outcomes. Ultimately, achieving optimal range of motion serves as a foundation for subsequent strengthening and functional exercises, paving the way for a safe and complete return to pre-injury activity levels.
4. Strengthening Exercises
Strengthening exercises form a cornerstone of posterior leaf of the oblique fibular ligament (plof) physical therapy, playing a crucial role in restoring ankle stability and function following injury. The plof, along with other lateral ankle ligaments, provides crucial support against excessive inversion (inward rolling) of the ankle. Injury to this ligament compromises this stability, increasing the risk of recurrent sprains and long-term dysfunction. Strengthening exercises target specific muscle groups that dynamically support the ankle joint, compensating for the compromised ligamentous support. These exercises focus primarily on the peroneal muscles, which run along the outer side of the lower leg and actively evert (outwardly rotate) the foot, counteracting inversion forces. For example, resisted ankle eversion exercises using resistance bands or weight machines directly strengthen the peroneals, enhancing their ability to stabilize the ankle. Additionally, strengthening exercises target the calf muscles (gastrocnemius and soleus), which contribute to overall ankle stability during weight-bearing activities.
The importance of strengthening exercises in plof physical therapy lies in their ability to improve dynamic stability, reduce the risk of re-injury, and enhance functional performance. A well-structured strengthening program not only improves muscle strength but also enhances neuromuscular control, the coordinated activation of muscles to maintain joint stability during movement. For example, exercises incorporating balance and proprioceptive challenges, such as single-leg stance exercises on unstable surfaces, improve neuromuscular control and enhance the ankle’s ability to react to perturbations and prevent reinjury. Furthermore, strengthening exercises improve the resilience of the ankle joint, enabling individuals to participate in higher-level activities without compromising stability. This is particularly important for athletes or individuals engaging in physically demanding occupations. The progressive nature of strengthening programs allows for gradual increases in load and complexity, facilitating a safe and effective return to pre-injury activity levels.
In summary, strengthening exercises are essential for successful outcomes in plof physical therapy. By targeting key muscle groups responsible for ankle stability, these exercises enhance dynamic support, improve neuromuscular control, and reduce the risk of recurrent injury. Challenges remain in determining the optimal exercise progression and intensity for individual patients. Ongoing research investigating the effectiveness of different strengthening protocols for plof injuries will further refine rehabilitation strategies. Ultimately, a comprehensive strengthening program, integrated with other components of plof physical therapy, is crucial for restoring optimal ankle function and facilitating a safe return to desired activities.
5. Proprioceptive Training
Proprioceptive training plays a critical role in posterior leaf of the oblique fibular ligament (plof) physical therapy by addressing the sensorimotor deficits that frequently accompany ankle injuries. Proprioception, the body’s ability to sense its position and movement in space, relies on specialized nerve receptors within muscles, tendons, and joints. Plof injuries, often occurring in conjunction with other ankle ligament sprains, can disrupt these neural pathways, leading to decreased joint position sense and impaired balance. This proprioceptive deficit increases the risk of recurrent ankle sprains and hinders functional recovery. Proprioceptive training aims to re-educate these sensorimotor pathways, enhancing joint stability and improving overall lower extremity function. For example, exercises involving balance boards, wobble cushions, or unstable surfaces challenge the ankle’s proprioceptive system, promoting improved joint position awareness and dynamic stability.
The practical significance of incorporating proprioceptive training within plof physical therapy lies in its ability to bridge the gap between basic strengthening exercises and functional activities. While strengthening exercises improve muscle strength and endurance, proprioceptive training enhances the neuromuscular control required for real-world movements. This translates to improved balance, agility, and coordination, reducing the risk of re-injury during activities such as walking on uneven terrain, changing direction quickly, or participating in sports. For instance, an athlete recovering from a plof injury might incorporate exercises like single-leg hops or agility drills on a balance beam to enhance proprioception and improve sport-specific performance. Furthermore, improved proprioception enhances the body’s natural protective mechanisms, allowing for quicker and more efficient responses to unexpected perturbations, thus minimizing the risk of future ankle injuries. This is particularly important for individuals with a history of ankle instability or those engaging in high-risk activities.
In conclusion, proprioceptive training serves as an essential component of comprehensive plof physical therapy. By addressing the sensorimotor deficits that often accompany these injuries, proprioceptive exercises enhance joint stability, improve balance, and reduce the risk of recurrent sprains. Challenges remain in quantifying proprioceptive improvements and developing standardized assessment tools. Ongoing research investigating the optimal dosage and progression of proprioceptive exercises for plof injuries will further refine rehabilitation protocols. Ultimately, incorporating proprioceptive training into plof physical therapy programs optimizes patient outcomes and facilitates a safe and successful return to pre-injury activity levels.
6. Functional activities
Functional activities represent a crucial bridge between therapeutic exercises and real-world demands within posterior leaf of the oblique fibular ligament (plof) physical therapy. These activities transition patients from isolated strengthening and range-of-motion exercises to movements that replicate daily or sport-specific actions. Plof injuries, often impacting ankle stability during weight-bearing activities, necessitate a rehabilitation approach that addresses functional limitations. Functional activities directly target these limitations, improving performance in tasks such as walking, stair climbing, running, jumping, or cutting maneuvers. For example, a patient recovering from a plof injury might progress from basic calf raises to performing single-leg hops or agility drills, thereby enhancing functional strength and stability in activities that mimic real-world demands. The incorporation of functional activities ensures that rehabilitation translates into tangible improvements in daily life or sport participation.
The importance of functional activities in plof physical therapy lies in their ability to address the specific biomechanical demands placed upon the ankle during dynamic movements. These activities require coordinated muscle activation, proprioceptive feedback, and adequate joint stabilityall essential components of functional ankle performance. For instance, a basketball player recovering from a plof injury would benefit from functional activities that replicate the demands of the sport, such as lateral shuffling, jumping, and landing. These activities challenge the ankle’s stability and neuromuscular control in a sport-specific context, ensuring a safe and effective return to play. Moreover, functional activities provide valuable feedback to both the patient and therapist, allowing for adjustments to the rehabilitation program based on individual progress and functional limitations. This individualized approach optimizes recovery and minimizes the risk of re-injury.
In summary, the integration of functional activities within plof physical therapy is essential for achieving optimal patient outcomes. These activities bridge the gap between isolated exercises and real-world demands, promoting a successful return to pre-injury activity levels. Challenges remain in defining standardized functional activity progressions for various patient populations and specific sports. Ongoing research investigating the effectiveness of different functional activity protocols will further enhance rehabilitation strategies for plof injuries. Ultimately, a focus on functional activities ensures that rehabilitation translates into meaningful improvements in patients’ lives, enabling them to regain their desired level of function and participate in the activities they enjoy.
7. Return to Activity
Return to activity represents the culmination of posterior leaf of the oblique fibular ligament (plof) physical therapy, signifying the successful restoration of ankle function and the patient’s ability to resume pre-injury activities. This phase of rehabilitation requires careful planning and individualized progression to minimize the risk of re-injury and ensure long-term success. A premature return to activity can exacerbate the initial injury, prolong recovery, and potentially lead to chronic ankle instability. Conversely, a well-structured return to activity program allows for gradual adaptation to increasing loads and demands, promoting tissue healing and enhancing functional capacity. For example, an athlete recovering from a plof injury might follow a phased return to sport protocol, beginning with low-impact activities like cycling or swimming before progressing to sport-specific drills and eventually full participation in training and competition. This gradual progression allows the repaired ligament and surrounding tissues to adapt to increasing stress, minimizing the risk of re-injury.
Several factors influence the timeline and progression of return to activity following a plof injury. The severity of the initial injury, individual healing capacity, and the specific demands of the intended activity all play a role. Objective measures such as range of motion, strength, and functional performance tests guide decision-making throughout this process. For instance, an individual demonstrating full range of motion, symmetrical strength compared to the uninjured limb, and the ability to perform sport-specific movements without pain or instability may be considered ready for a progressive return to activity. Furthermore, communication between the patient, therapist, and physician (if applicable) is essential to ensure a safe and effective transition back to desired activity levels. Collaboration among these stakeholders ensures that individual needs and goals are considered, maximizing the likelihood of a successful outcome. For those involved in competitive sports, specialized testing and performance evaluations may be necessary to ensure readiness for the high demands of competition.
In summary, return to activity signifies successful rehabilitation following a plof injury. A well-structured, individualized approach minimizes re-injury risk and maximizes long-term functional outcomes. Challenges remain in defining standardized return to activity criteria for various patient populations and specific activities. Ongoing research investigating optimal return to activity protocols will further refine rehabilitation strategies and improve patient outcomes. Effective communication and collaboration among healthcare professionals and patients remain essential for achieving a safe and successful return to pre-injury activity levels.
Frequently Asked Questions about Posterior Leaf of Oblique Fibular Ligament (plof) Physical Therapy
This section addresses common questions regarding rehabilitation for posterior leaf of the oblique fibular ligament (plof) injuries.
Question 1: How long does plof physical therapy typically last?
Recovery timelines vary based on injury severity and individual healing rates. Generally, rehabilitation can range from several weeks to a few months. Factors such as adherence to the prescribed program, the presence of other associated injuries, and individual healing capacity influence the overall duration of therapy.
Question 2: What are the signs that a plof injury might require surgical intervention?
Persistent instability, significant pain despite conservative treatment, or evidence of a complete ligament tear on imaging studies may warrant surgical consultation. A qualified orthopedic surgeon can determine the appropriateness of surgical intervention based on individual circumstances.
Question 3: Are there specific activities to avoid during plof physical therapy?
Activities that stress the lateral ankle ligaments, such as cutting or pivoting movements, should generally be avoided during the initial phases of rehabilitation. Specific activity restrictions will be determined based on individual injury status and progression through the rehabilitation program. Gradual reintroduction of activities under the guidance of a physical therapist minimizes re-injury risk.
Question 4: What are the potential long-term consequences of an untreated plof injury?
Untreated plof injuries can lead to chronic ankle instability, recurrent sprains, persistent pain, and decreased functional capacity. Early diagnosis and appropriate intervention, including physical therapy, are crucial for preventing these long-term complications.
Question 5: How can one differentiate a plof injury from a typical ankle sprain?
Differentiating a plof injury from other ankle sprains can be challenging and often requires specialized clinical examination and imaging. Localized tenderness along the course of the plof, combined with specific stability tests, may suggest a plof injury. Magnetic resonance imaging (MRI) can provide definitive confirmation and assess the extent of ligament damage.
Question 6: What can be expected during a typical plof physical therapy session?
A typical session might include pain management modalities (e.g., ice, ultrasound), manual therapy techniques, range-of-motion exercises, strengthening exercises, and proprioceptive training. The specific components of each session will be tailored to the individual’s needs and progress through the rehabilitation program.
Understanding these common concerns empowers individuals to actively participate in their rehabilitation and achieve optimal outcomes following a plof injury. It’s essential to consult with qualified healthcare professionals for personalized guidance and treatment plans.
The following section delves into advanced diagnostic and treatment techniques for plof injuries.
Conclusion
This exploration of posterior leaf of oblique fibular ligament (plof) physical therapy has highlighted the critical role of comprehensive rehabilitation in restoring ankle stability and function following injury. From initial diagnosis and pain management to strengthening, proprioceptive training, and functional activity progression, each component contributes significantly to successful outcomes. Addressing plof injuries requires a nuanced understanding of ankle biomechanics, accurate assessment, and individualized treatment planning. The information presented underscores the importance of early intervention and diligent adherence to prescribed rehabilitation protocols.
Effective plof physical therapy management minimizes the risk of chronic ankle instability, recurrent sprains, and long-term functional limitations. Further research investigating optimal rehabilitation strategies and diagnostic techniques will continue to refine treatment approaches and improve patient outcomes. Ultimately, prioritizing appropriate and timely plof physical therapy interventions promotes optimal recovery and enables individuals to regain their desired activity levels, minimizing the impact of these injuries on long-term ankle health and overall well-being.