Chapter 6 in a typical radiographic physics and imaging textbook commonly covers the principles of radiographic image formation and quality. This encompasses topics such as beam geometry, spatial resolution, receptor characteristics, image contrast, and the factors influencing these elements. Practical examples often include diagrams of beam projections, illustrations of image artifacts, and graphs demonstrating the relationship between exposure factors and image quality.
A thorough understanding of these concepts is fundamental for radiographers to produce diagnostic-quality images. Manipulating factors like milliampere-seconds (mAs), kilovoltage peak (kVp), source-to-image distance (SID), and object-to-image distance (OID) directly impacts image characteristics. Historically, advancements in understanding these principles have driven improvements in image quality, reducing patient dose, and expanding the diagnostic capabilities of radiography. Optimizing these parameters minimizes repeat exposures, benefiting both patient safety and departmental efficiency.
Further exploration of this subject typically involves detailed discussions of specific image quality factors, including sharpness, distortion, and noise. Additional topics may encompass the effects of scattered radiation, grids, and the principles of digital image processing.
Tips for Optimizing Radiographic Image Quality
The following tips offer practical guidance for applying principles of radiographic image formation and enhancing image quality. These recommendations aid in producing diagnostic images while minimizing patient dose.
Tip 1: Optimize mAs and kVp: Careful selection of milliampere-seconds (mAs) and kilovoltage peak (kVp) is crucial. Adequate mAs ensures sufficient radiation reaches the receptor for optimal image density, while appropriate kVp controls the penetrating power of the x-ray beam and influences subject contrast.
Tip 2: Maintain Proper SID: Adhering to the correct source-to-image distance (SID) is essential for minimizing magnification and geometric distortion. Variations in SID can significantly impact image sharpness and accuracy of size representation.
Tip 3: Minimize OID: Reducing object-to-image distance (OID) helps to sharpen images and reduce magnification. Positioning the anatomical area of interest as close to the image receptor as possible is crucial for optimal image quality.
Tip 4: Employ Effective Collimation: Precise collimation restricts the x-ray beam to the area of interest, minimizing patient dose and reducing scattered radiation, which degrades image contrast.
Tip 5: Utilize Grids Appropriately: Grids absorb scattered radiation before it reaches the image receptor. Using grids is particularly important for thicker body parts where scatter production is more significant.
Tip 6: Select Appropriate Image Receptors: Choosing the correct image receptor, whether film-screen or digital, influences spatial resolution and contrast characteristics. Receptor selection should be based on the specific examination being performed.
Tip 7: Implement Proper Patient Positioning: Accurate patient positioning ensures that the anatomy of interest is correctly projected onto the image receptor, avoiding overlapping structures and optimizing image interpretation.
By adhering to these principles, radiographers can significantly enhance image quality, leading to more accurate diagnoses and improved patient care. Implementing these practices contributes to radiation dose reduction, ensuring patient safety and optimizing departmental efficiency.
These practical applications of radiographic principles form the foundation for advanced imaging techniques and further study in the field.
1. Image Formation
Image formation is a core concept within radiographic physics and imaging, typically emphasized in Chapter 6 of foundational texts. Understanding the processes involved in creating a radiographic image is essential for producing diagnostic-quality results and interpreting them accurately. This section explores the facets of image formation, relating them to the broader context of radiographic principles.
- Differential Absorption
Differential absorption is the fundamental principle underlying image formation. X-rays passing through the patient are attenuated to varying degrees depending on the tissue density and atomic number of the structures they encounter. Denser tissues, such as bone, absorb more x-rays, resulting in lighter areas on the image. Less dense tissues, such as lung tissue, absorb fewer x-rays, resulting in darker areas. This variation in x-ray absorption creates the contrast necessary to visualize anatomical structures. The degree of differential absorption is directly influenced by the selected kVp.
- Beam Geometry
The geometry of the x-ray beam plays a critical role in image formation, influencing factors like magnification, distortion, and spatial resolution. The source-to-image distance (SID) and object-to-image distance (OID) are key geometric parameters. A longer SID minimizes magnification, while a shorter OID reduces both magnification and geometric distortion. Understanding and controlling these parameters is essential for accurate image representation.
- Scatter Radiation
Scatter radiation arises from the interaction of x-rays with matter, specifically through Compton scattering. Scattered photons deviate from their original path, contributing to overall image fog and reducing contrast. Managing scatter radiation through techniques like collimation and grid use is vital for optimizing image quality. The amount of scatter radiation produced is influenced by factors like patient thickness and kVp.
- Image Receptors
Image receptors capture the transmitted x-ray beam and convert it into a visible image, either directly in digital systems or indirectly through a latent image in film-screen systems. The characteristics of the receptor, including its sensitivity, resolution, and dynamic range, directly impact the final image quality. The choice of receptor depends on the specific imaging application and desired image characteristics.
These interconnected facets of image formation are integral to understanding Chapter 6 principles. Manipulating factors influencing differential absorption, beam geometry, scatter radiation, and receptor characteristics allows radiographers to optimize image quality, minimize patient dose, and ensure diagnostic accuracy. A thorough understanding of these principles provides the foundation for advanced imaging techniques and interpretation.
2. Beam Geometry
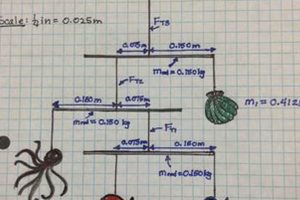
Beam geometry is a critical component within the broader context of radiographic physics and imaging, typically a core topic in Chapter 6 of introductory texts. A thorough understanding of beam geometry is essential for producing diagnostic-quality radiographic images, as it directly influences image sharpness, magnification, and distortion. This section explores the key facets of beam geometry as they relate to image formation and interpretation.
- Source-to-Image Distance (SID)
SID refers to the distance between the x-ray source (focal spot) and the image receptor. Increasing the SID minimizes magnification and improves spatial resolution, creating a sharper image. Conversely, a shorter SID increases magnification and can lead to geometric blurring. Standardized SIDs are used in various radiographic procedures to ensure consistent image quality.
- Object-to-Image Distance (OID)
OID represents the distance between the object being imaged and the image receptor. Minimizing OID is crucial for reducing both magnification and geometric unsharpness. Placing the anatomical area of interest as close to the receptor as possible is a standard practice to optimize image quality. Increased OID contributes to image blurring and misrepresentation of the true size of the anatomical structures.
- Focal Spot Size
The focal spot size of the x-ray tube directly impacts image sharpness. A smaller focal spot produces sharper images with finer detail, while a larger focal spot can lead to increased penumbra and blurring. The selection of the appropriate focal spot size depends on the desired level of detail and the heat-loading capacity of the x-ray tube.
- Central Ray Alignment
The central ray (CR) is the central portion of the x-ray beam. Proper alignment of the CR with the anatomical area of interest and the image receptor is essential for minimizing shape distortion. Angulation of the CR can be used intentionally to project superimposed anatomical structures for specific diagnostic purposes, but unintentional misalignment can lead to inaccurate representation of anatomy.
These interconnected facets of beam geometry are integral to understanding Chapter 6 principles. Manipulating SID, minimizing OID, selecting the appropriate focal spot size, and ensuring accurate CR alignment are essential skills for radiographers. Mastering these principles enables the production of high-quality diagnostic images and minimizes unnecessary patient radiation exposure. This foundation in beam geometry underpins more advanced imaging techniques and interpretation skills.
3. Spatial Resolution
Spatial resolution, a core concept explored in “essentials of radiographic physics and imaging chapter 6,” refers to the ability of an imaging system to distinguish between two closely spaced objects. High spatial resolution allows for visualization of fine details and subtle changes in anatomical structures, which is crucial for accurate diagnosis. This characteristic is quantified by the number of line pairs per millimeter (lp/mm) that can be distinguished in an image. Several factors influence spatial resolution, and understanding their interplay is crucial for optimizing image quality.
- Focal Spot Size
The focal spot size of the x-ray tube has a direct impact on spatial resolution. A smaller focal spot produces a sharper image with better resolution, as it minimizes the area from which x-rays originate, reducing geometric blurring (penumbra). Conversely, a larger focal spot results in greater penumbra and reduced sharpness. Choosing the appropriate focal spot size depends on the balance between desired resolution and the heat-loading capacity of the x-ray tube.
- Source-to-Image Distance (SID)
Increasing the SID improves spatial resolution by minimizing magnification and geometric blurring. A longer SID leads to a more parallel x-ray beam, reducing the penumbra effect and resulting in a sharper image. Standardized SIDs are implemented in radiographic procedures to maintain consistent image quality and optimize resolution.
- Object-to-Image Distance (OID)
Minimizing OID is crucial for enhancing spatial resolution. A smaller OID reduces magnification and geometric unsharpness, leading to a clearer and more detailed image. Positioning the anatomical structure of interest as close to the image receptor as possible is essential for optimal resolution.
- Motion Blur
Motion, either from the patient or the imaging equipment, significantly degrades spatial resolution. Patient motion can be minimized through clear communication, proper immobilization techniques, and short exposure times. Equipment motion, although less common, can also contribute to blurring and should be addressed through regular maintenance and quality control procedures.
These factors, all discussed within the context of “essentials of radiographic physics and imaging chapter 6,” interact to determine the overall spatial resolution of a radiographic image. Optimizing these parameters is essential for maximizing diagnostic information and ensuring accurate image interpretation. The ability to visualize fine anatomical details, made possible by high spatial resolution, is crucial for detecting subtle pathologies and providing optimal patient care.
4. Receptor Characteristics
Receptor characteristics are integral to understanding radiographic image formation, a key topic within “essentials of radiographic physics and imaging chapter 6.” These characteristics significantly influence the quality and diagnostic value of radiographic images. A comprehensive understanding of receptor types and their performance parameters is fundamental for optimizing image acquisition and interpretation.
- Absorption Efficiency
Absorption efficiency describes the receptor’s ability to absorb incident x-ray photons. Higher absorption efficiency results in a greater percentage of the x-ray beam being utilized for image formation, contributing to improved image quality and reduced patient dose. This characteristic varies depending on the receptor material and thickness and is crucial for both film-screen and digital systems.
- Conversion Efficiency
Conversion efficiency refers to the ability of the receptor to convert absorbed x-ray energy into a usable signal. In digital systems, this involves converting x-ray photons into electrons, which are then digitized to form the image. In film-screen systems, the absorbed energy converts into light photons, which expose the film. Higher conversion efficiency contributes to improved image quality and reduced patient dose.
- Spatial Resolution
Spatial resolution describes the receptor’s ability to distinguish between two closely spaced objects. High spatial resolution is crucial for visualizing fine details and subtle anatomical changes. This characteristic is typically quantified in line pairs per millimeter (lp/mm) and is influenced by factors such as detector element size in digital systems and phosphor crystal size in film-screen systems. Higher spatial resolution contributes to improved diagnostic accuracy.
- Dynamic Range
Dynamic range represents the range of x-ray exposures that a receptor can accurately capture and represent in the image. Digital receptors generally have a wider dynamic range compared to film-screen systems, allowing for visualization of both dense and lucent structures within the same image without significant loss of detail. A wide dynamic range is essential for optimizing image quality across a variety of anatomical regions and examination types.
These interconnected receptor characteristics, explored in “essentials of radiographic physics and imaging chapter 6,” are crucial for achieving optimal image quality. Understanding the specific properties of different receptor types, including their absorption efficiency, conversion efficiency, spatial resolution, and dynamic range, allows radiographers to tailor imaging techniques to specific clinical needs and maximize diagnostic information while minimizing patient dose.
5. Image Contrast
Image contrast, a core component of “essentials of radiographic physics and imaging chapter 6,” refers to the difference in brightness between various regions of a radiographic image. Adequate contrast is essential for distinguishing anatomical structures and making accurate diagnoses. This section explores the factors influencing image contrast and their impact on image quality.
- Subject Contrast
Subject contrast refers to the inherent differences in x-ray attenuation between tissues within the patient. Factors such as tissue thickness, density, and atomic number contribute to subject contrast. Tissues with higher atomic numbers, like bone, attenuate more x-rays and appear brighter on the image compared to tissues with lower atomic numbers, like lung tissue. Manipulating kilovoltage peak (kVp) influences subject contrast. Lower kVp generally enhances subject contrast, while higher kVp reduces it.
- Scatter Radiation
Scatter radiation, arising from Compton interactions within the patient, degrades image contrast by adding a uniform fog to the image. This fog reduces the difference in brightness between adjacent structures, making them less distinct. Techniques like collimation and the use of grids help minimize scatter radiation and improve image contrast. Grids are particularly important when imaging thicker body parts, where scatter production is more significant.
- Kilovoltage Peak (kVp)
kVp significantly influences image contrast by affecting the energy of the x-ray beam. Higher kVp produces a more penetrating beam with a wider range of energies, leading to a reduction in subject contrast. Lower kVp results in a less penetrating beam and enhances subject contrast, although it increases patient dose. Selecting the appropriate kVp requires a balance between achieving adequate contrast and minimizing patient exposure.
- Image Receptor Characteristics
The characteristics of the image receptor, whether film-screen or digital, also influence the final contrast displayed in the image. Digital receptors generally offer a wider dynamic range compared to film-screen systems, contributing to improved contrast visualization. The receptor’s inherent contrast characteristics play a significant role in the overall image quality.
These interconnected factors, discussed within the context of “essentials of radiographic physics and imaging chapter 6,” collectively determine the final image contrast. Optimizing these parameters, including managing scatter radiation, selecting appropriate kVp, and considering receptor characteristics, are crucial for maximizing diagnostic information and ensuring accurate image interpretation. Appropriate image contrast is fundamental for visualizing subtle anatomical details and facilitating effective patient care.
6. Scattered Radiation
Scattered radiation is a critical topic within the context of “essentials of radiographic physics and imaging chapter 6,” representing a significant challenge in producing diagnostic-quality radiographic images. It arises from the interaction of the primary x-ray beam with matter, specifically through Compton scattering. In this process, an incident x-ray photon interacts with an outer-shell electron, losing some energy and changing direction. This scattered radiation, deviating from the original beam path, contributes to image degradation by reducing contrast and adding an overall fog. Understanding its origins and effects is crucial for optimizing image quality and minimizing patient dose.
The degree of scatter production depends on several factors, including patient thickness, field size, and kilovoltage peak (kVp). Thicker body parts generate more scatter due to increased opportunities for interaction. Larger field sizes also contribute to increased scatter. Higher kVp increases the likelihood of Compton interactions, leading to a greater proportion of scattered photons. For example, a chest x-ray of a larger patient will produce more scatter than a hand x-ray of a smaller patient due to the increased tissue volume and likely higher kVp used. This scatter reduces the contrast between lung tissue and surrounding structures, making it more challenging to discern subtle details. In a hand x-ray, the lower scatter allows for better visualization of fine bone structures.
Managing scattered radiation is essential for producing diagnostic images. Two primary methods employed are collimation and the use of grids. Collimation restricts the x-ray beam to the area of interest, reducing the volume of tissue irradiated and thus minimizing scatter production. Grids, placed between the patient and the image receptor, consist of lead strips that absorb scattered photons while allowing the primary beam to pass through. Effective use of these techniques is crucial for improving image contrast and ensuring diagnostic accuracy. Addressing scatter radiation is fundamental for optimizing image quality and minimizing unnecessary patient exposure, aligning with the core principles presented in “essentials of radiographic physics and imaging chapter 6.” Understanding these principles and applying appropriate techniques improves the diagnostic value of radiographic images and contributes to better patient care.
7. Digital Image Processing
Digital image processing is integral to modern radiography, representing a significant advancement in the field and a key topic within “essentials of radiographic physics and imaging chapter 6.” It encompasses a range of computational techniques applied to digital radiographic images to enhance their diagnostic quality. These processes optimize image display for interpretation, contributing significantly to accurate diagnoses. Understanding these techniques is fundamental for radiographers working with digital imaging systems.
- Preprocessing
Preprocessing techniques address imperfections inherent in the image acquisition process. These corrections compensate for variations in receptor sensitivity and electronic noise, ensuring a uniform and consistent image. For instance, flat-field correction compensates for variations in pixel response across the detector, resulting in a more uniform image background. This is crucial for accurate diagnosis, as uncorrected variations could be misinterpreted as pathological findings. Within the context of “essentials of radiographic physics and imaging chapter 6,” preprocessing ensures that the acquired image accurately represents the attenuated x-ray beam, providing a reliable foundation for subsequent processing and interpretation.
- Contrast Enhancement
Contrast enhancement techniques modify the image histogram to optimize the display of anatomical details. These adjustments can increase the difference in brightness between areas of interest and surrounding tissues, improving visibility. For example, windowing and leveling allow adjustment of the displayed image contrast and brightness to highlight specific anatomical features. In chest radiography, specific windowing settings can optimize the visualization of lung tissue versus mediastinal structures. This relates directly to the principles of image contrast discussed in “essentials of radiographic physics and imaging chapter 6,” where understanding contrast manipulation is essential for diagnostic interpretation.
- Spatial Frequency Filtering
Spatial frequency filtering techniques modify the sharpness and detail within the image by manipulating the frequency components of the image data. Edge enhancement filters accentuate high-frequency components, improving the visibility of fine details and edges. Smoothing filters reduce noise and blur by suppressing high-frequency components. For example, edge enhancement can be beneficial in mammography for visualizing microcalcifications, while smoothing filters can reduce noise in low-dose imaging. This relates to the principles of spatial resolution covered in “essentials of radiographic physics and imaging chapter 6,” demonstrating how digital processing can enhance the inherent resolution capabilities of the imaging system.
- Digital Subtraction Angiography (DSA)
Digital subtraction angiography (DSA) is a specialized technique used to visualize blood vessels. A pre-contrast image is acquired, followed by a series of images acquired after the injection of a contrast agent. By digitally subtracting the pre-contrast image from the post-contrast images, the bones and other surrounding tissues are removed, leaving a clear visualization of the contrast-filled vessels. This technique relies on precise image registration and subtraction algorithms. DSA exemplifies a sophisticated application of digital image processing, building upon the foundational principles of image acquisition and contrast manipulation covered in “essentials of radiographic physics and imaging chapter 6.”
These digital image processing techniques, explored within the context of “essentials of radiographic physics and imaging chapter 6,” are essential tools for enhancing the diagnostic value of radiographic images. They represent a significant advancement in the field, enabling optimization of image display, improved visualization of anatomical details, and ultimately, more accurate and timely diagnoses. These techniques directly relate to and expand upon the fundamental principles of radiographic image formation discussed in Chapter 6, demonstrating how digital technologies have revolutionized image acquisition and interpretation in modern radiology.
Frequently Asked Questions
This section addresses common queries regarding fundamental principles of radiographic image formation and quality, often covered in chapter 6 of standard radiographic physics and imaging texts. Clarifying these concepts is crucial for a comprehensive understanding of image acquisition and interpretation.
Question 1: How does kilovoltage peak (kVp) affect image contrast?
Higher kVp produces a more penetrating x-ray beam with a wider range of energies, resulting in lower subject contrast. Conversely, lower kVp enhances subject contrast but increases patient dose.
Question 2: What is the impact of source-to-image distance (SID) on image magnification?
Increasing SID minimizes magnification and improves spatial resolution, while decreasing SID increases magnification and can reduce image sharpness.
Question 3: How does scattered radiation degrade image quality?
Scattered radiation reduces image contrast by adding a uniform fog, making it more difficult to distinguish between adjacent anatomical structures. This necessitates strategies like collimation and grid use to minimize scatter.
Question 4: What is the significance of object-to-image distance (OID) in image formation?
Minimizing OID reduces both magnification and geometric unsharpness, contributing to a clearer and more accurate representation of the anatomical area of interest.
Question 5: How do digital image receptors differ from film-screen systems in terms of dynamic range?
Digital receptors typically exhibit a wider dynamic range than film-screen systems, allowing for visualization of a broader range of tissue densities within a single image without significant loss of detail.
Question 6: What is the role of spatial resolution in diagnostic imaging?
Spatial resolution, the ability of an imaging system to distinguish between closely spaced objects, is crucial for visualizing fine details and subtle anatomical changes, directly impacting diagnostic accuracy.
Understanding these fundamental principles is essential for optimizing image quality, minimizing patient dose, and ensuring accurate image interpretation. This knowledge forms the foundation for advanced imaging techniques and contributes significantly to effective patient care.
Further exploration of these topics may involve detailed examination of specialized imaging techniques, image artifacts, and quality control procedures.
Conclusion
Mastery of the principles presented in resources like “essentials of radiographic physics and imaging chapter 6” is crucial for competent radiographic practice. This knowledge base, encompassing image formation, beam geometry, spatial resolution, receptor characteristics, image contrast, scatter radiation, and digital image processing, empowers radiographers to consistently produce high-quality diagnostic images. A thorough understanding of these interconnected concepts enables informed decision-making regarding technique selection, optimization of image acquisition parameters, and accurate image interpretation.
Continued advancements in imaging technology necessitate ongoing engagement with these foundational principles. As imaging modalities evolve and new techniques emerge, a strong grasp of these core concepts remains essential for adapting to innovations and ensuring optimal patient care through accurate and efficient image acquisition and interpretation. Dedication to lifelong learning and professional development in radiographic physics and imaging is paramount for maintaining competency and advancing the field.